Article • Breast cancer detection
New DNA test could prevent thousands of mastectomies
A new genetic test to assess breast cancer risk in women who have a family history of the disease could be introduced into clinical practice in the UK within the next few months.
Report: Mark Nicholls

Devised at Manchester University NHS Foundation Trust (MFT) and the University of Manchester, researchers believe the test for high-risk groups could also help reduce the number of women needing to have surgery to remove their breasts. By narrowing down their risk, women will be better informed about whether to have a mastectomy, or not, explained Professor Gareth Evans, who led the work that resulted in the new test. Scientists say the test will accurately predict breast cancer risk in women who do not test positive for BRCA1/2 gene mutations and, in some cases, may also help to refine breast cancer risk in those with the BRCA1/2 mutations.
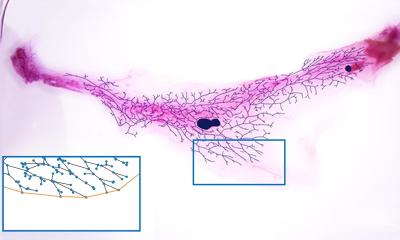
The most common cancer that affects women having a parent or sibling with breast cancer makes women twice as likely to develop breast cancer themselves. Mutations in the BRCA1/2 genes have been identified as a cause of hereditary cancer, but only account for 15-20% of the underlying inherited genetic trigger for the condition. The new genetic test assesses breast cancer risk based on genetic variations - single nucleotide polymorphisms (SNPs) - in an individual’s DNA. Researchers found that mutations of 18 SNPs were indicative of breast cancer risk for women who did not carry BRCA1/2 mutations. These were found to have minimal effect in isolation, but when combined could increase or decrease breast cancer risk considerably.
The study recruited 451 women (112 with BRCA1/2 mutations) with a family history of breast cancer who had developed breast cancer. The researchers compared the diagnosis of invasive breast cancer and genetic profile in the case group against that of a control group of 1,605 women (691 with BRCA1/2 mutations). The analysis of DNA using participants’ blood samples was used to determine their individual genetic makeup and predict an overall risk estimate alongside other risk factors such as age at first assessment, family history of first and second-degree relatives, age at first child, first period and menopause, height and weight, and history of prior non-cancerous breast disease.
From the findings, women originally viewed as at high risk (lifetime risk of 30% or greater) were reclassified to a lower risk, where mastectomy is not recommended to reduce the risk. The study suggested that the number of women with BRCA1/2 mutations who currently choose to have a mastectomy could now fall by a third from 50% to 36%.
We plan to develop new screening strategies and biomarkers for other common cancers, including womb, bowel, ovarian and prostate
Gareth Evans
Professor Evans, a Consultant in Medical Genetics and Cancer Epidemiology at The University of Manchester and the city’s Saint Mary’s Hospital – where the test will first be made available – said: ‘This new test will help women at risk of familial breast cancer to make more informed decisions about their care. ‘BRCA1 and BRCA2 are just part of what we should be looking for when assessing risk and in Manchester we plan to incorporate screening for these new genetic markers in clinical practice within the next six months. ‘We are committed to improving cancer prevention through research and, with funding from the NIHR Manchester Biomedical Research Centre, we plan to develop new screening strategies and biomarkers for other common cancers, including womb, bowel, ovarian and prostate.’ Professor Evans is hoping the test will become more widely available, and describes it as a ‘massive game changer for breast cancer’, which can accurately assess risk in the whole population from those with a family history and those with BRCA mutations.
Profile:
Gareth Evans is Professor of Medical Genetics and Cancer Epidemiology at the University of Manchester, UK, and Consultant in Medical Genetics and Cancer Epidemiology, Central Manchester Hospitals NHS Foundation Trust and The Christie NHS Foundation Trust. He has an international reputation in clinical and research aspects of cancer genetics, particularly in neurofibromatosis and breast cancer, in which his group is particularly interested in biomarkers that indicate the risk of developing breast cancer.
15.12.2017