Neuro Imaging
Molecular imaging brings seismic change
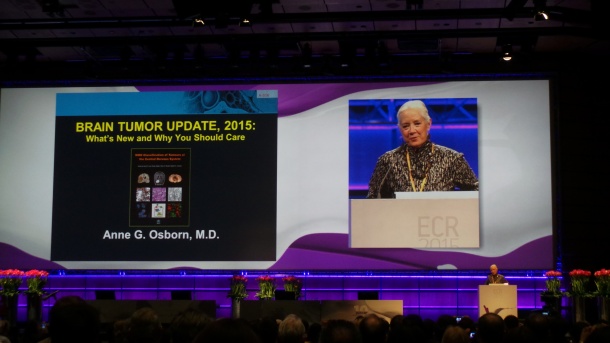
Molecular profiling is transforming brain cancer management and radiologists must get to grips with the upcoming paradigm that will affect the way they report findings. Renowned neuroradiologist Professor Anne G. Osborn from the University of Utah, School of Medicine, Salt Lake City, unveiled the latest advances in brain pathology during the Nikola Tesla Honorary Lecture last week at ECR 2015.
Report: Mélisande Rouger
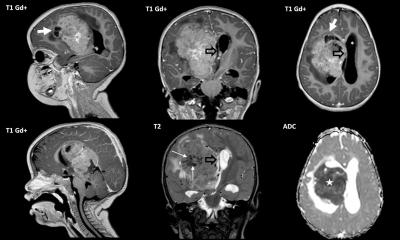
Osborn focused on atypical teratoid/rhaboid tumours (AT/RT) and medulloblastoma (MB) tumours, as well as diffusedly infiltrating gliomas and paediatric brain stem gliomas. AT/RT are one of the most lethal or aggressive childhood brain tumours; they have very specific gene deletion INI1, which is now considered diagnostic of these tumours. “Using the phenotypes of these tumours, pathologists would say: ok, it is a large, fleshy tumour where haemorrhage and necrosis are common. Using a microscopic analysis, it is interesting because they have large pale cells but they often do not have overtly rhaboid phenotypes. However loss of nuclear staining for INI1 is now pathognomonic for this type of tumour - so neither the phenotype nor the microscopic appearance, but its genotype,” she said.
Neuropathologists are going to create layers of diagnosis, and the most specific diagnosis is going to be the one that uses molecular information, according to Osborn. “It is important for stratifying patients for tumour treatment, and particularly important with other types of tumours like MBs and gliomas,” the expert pointed out.
MB is perhaps the best known tumour in which the genotype is superseding or trumping the phenotype information. According to the old phenotypic classification, there is classical MB and three variants: the desmoplastic MB, MB with extensive nodularity and anaplastic or large cell MB. “They look a lot like small round blue cell tumours, you have all seen these kinds of tumours,” she said.
In the last two years, it has become very apparent that MB is not a single disease; it has a lot of variation on its biological behaviour, sometimes it behaves well, sometimes it does not. According to molecular profiling, there are four different MB tumours, each of which has different risks, and each of which may be treated differently. “Molecular profiling or genomic information is now the first step in stratifying the patient for risk and prognosis and treatment,” she said.
The four recognized molecular subgroups are the SHH (sonic hedgehog) and Wnt (wingless) pathways, and two non-SHH and non-Wnt subtypes named Group 3 and Group 4, in the absence of better names. Some imaging correlates can give a clue as to the phenotypic or genotypic type. The SHH subgroup is the second largest group of MBs, and is typically more common in the lateral cerebellum than in the midline. “If it´s in the lateral cerebellum and has solid enhancement, most of these are going to SHH,” Osborn stated. Wnt may be the smallest group of MBs but is has the best prognosis; more than 90% of these patients will survive in the long term. An imaging surrogate marker for these tumours is their typical location in the CPA or cerebellar peduncle. This information is significant because, since it has very good prognosis, children may be spared chemotherapy and only undergo surgery. Group 3 MBs have terrible survival and most of them are located right in the midline. However there is nothing that distinguishes them on imaging as of today. Group 4 MBs have intermediate survival and are mainly present in the midline; they tend to have minimal or no enhancement.
Radiogneomic surrogate markers have changed our understanding of MBs, Osborn pointed out. “MBs have been called by definition very bad tumours with terrible prognosis. But we now know that this is going to be misleading for the Wnt blastomas, as their prognosis is much better and their treatment will be different from the other MBs. So it may be that they will be called not grade 4, but maybe grade 2,” she explained. She then took a look at gliomas, which were named for the cells they look like. It was long thought that tumours arose in the brain when one of these mature cells went bad, but researchers now know that it isn´t the case and that they probably arise from plutripotential stem cells.
The Cancer Genome Atlas shows that gliomas are remarkably complex and heterogeneous tumours. They may have more than one cell type, and even the genotype may change as they progress and recur. Neuropathologists are now calling neuroplastomas not multiforme but only glioblastoma, so radiologists must take that into consideration. There are four distinct molecular subtypes of GBMs: three preneural and one classical and each has prognostic and treatment implications.
Researchers now agree that primary GBMs are the most common, are typically characterised by IDH1- and have poor prognosis. The secondary GBMs arise from lower grade tumours, are mainly IDH1+ and have better prognosis. In terms of imaging surrogate markers, GBMs appear to be typically present in the frontal lobe and have large non-enhancing areas.
Regarding low-grade gliomas, the old thinking was that they were six histopathologically recognised LGGs, now they are going to be defined by only three molecular subtypes. They are based on IDH, 1p19q and ATRX status. “In conclusion, we are looking at a seismic change in the way pathologists are looking at brain tumour. All of basic physiologic, histologic and phenotypic information is going to be meaningless because the genetic is what is going to count. We are going to integrate our genomics into imaging if we are aware of the integrated layered diagnosis and know that, for example in MB, the location and enhancement patterns can help us saying what type of MB it is,” she concluded.
07.03.2015