Article • To-Be for tomo
Two-part trial studies tomosynthesis benefits
The UNESCO World Heritage City Bergen is seen as the gateway to the fiords of Norway. However, for radiologists the city offers an even more interesting attraction than Scandinavian landscapes. Bergen features one of the largest randomised control trials to compare digital breast tomosynthesis (DBT) with digital mammography (DM): the To-Be trial. Professor Solveig Hofvind, head of BreastScreen Norway, outlined the study and its promising interim results at ECR 2018.
Report: Lena Petzold

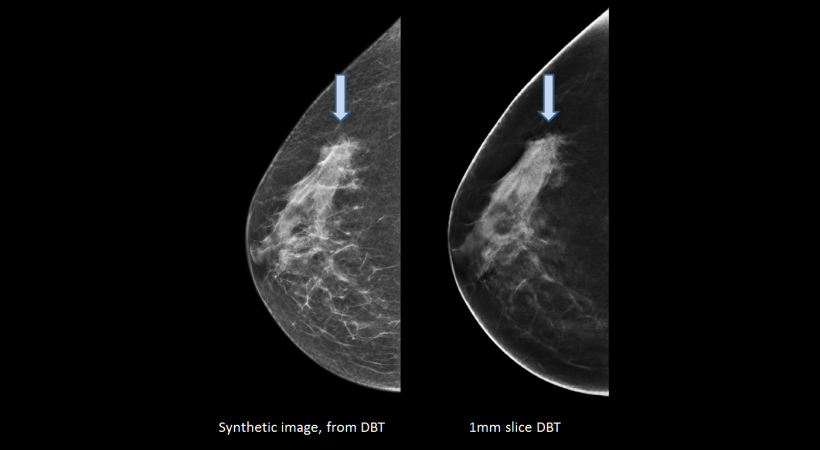
‘There were several reasons why we wanted to start this specific trial,’ Professor Solveig Hofvind says, to explain the value of the To-Be trial. ‘A number of studies have already shown a higher cancer detection rate for tomosynthesis compared to digital mammography. However, most of these used DM in addition to DBT, which meant doubling the radiation dose for women. Furthermore, many studies were performed in the USA in a much broader range. ‘We wanted to compare DBT and synthetic 2-D mammograms against digital mammography in a screening setting featuring European specifics and matching the gold standard criteria,’ she says, and underlines that the European perspective is especially important when it comes to recall rates. ‘The USA recall rate is between ten and fifteen per cent, whilst in Europe it is between three and five percent. Although the rate reduction through tomosynthesis is a great achievement for women in the States, it is a much more difficult task to achieve in Europe and should therefore be studied separately.’
A great advantage of the trial is that the study group has access to important follow-up clinical data of more than 99.9 per cent of their participating patients. All women diagnosed with breast cancer in Norway are included in the Norwegian cancer registry, so the group can access this data for their participants and closely follow their progress.
To-Be 1
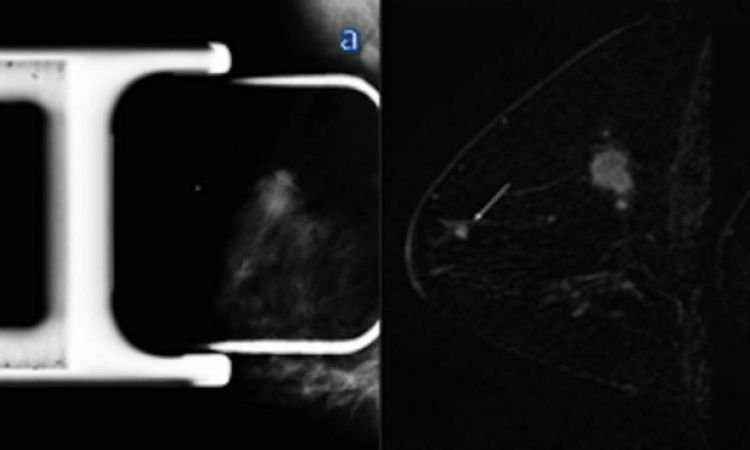
The To-Be trial consists of two parts. In To-Be 1, DBT and synthetic 2-D mammograms are tested against digital mammography in a screening setting using equipment from GE Healthcare.
All women in Norway age 50 to 69 are offered a mammography screening every two years. The attendance rate per screening round is 75 percent, so the coverage is very high, Hofvind confirms. Norway has 30 screening units, but only one in Bergen. For To-Be 1, all women who attended the breast screening unit in Bergen in 2016 and 2017 were asked about participation. Those who said ‘yes’ signed an informed consent and were electronically randomised into digital mammography or tomosynthesis afterwards. The participation rate was close to 90 percent; so about 30,000 women were screened. ‘In Norway we do independent double reading with consensus or arbitration, as in most European countries,’ the expert adds.
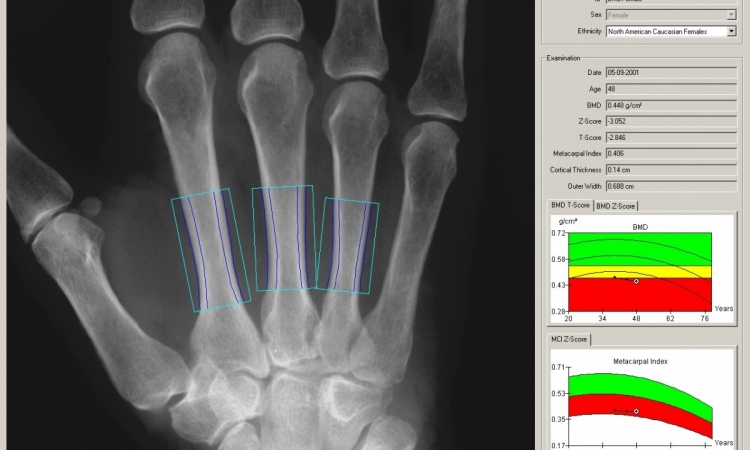
The aim of To-Be 1 is to compare the early screening outcome and economic cost of screening with DBT vs. DM in a population-based screening program. The interim analysis focuses on interpretation time, consensus and recall rate as well as on the stratification of data by mammographic density measured via an automated system. ‘We also want to look at the rate of interval cancers detected between two screening rounds. Therefore we have to wait two years after the last woman was screened for the data to become available.’
To specifically determine the cost of DBT vs. DM, the study team coded every process step, from time spent on consensus to diagnostics, as well as treatment per screen-detected cancer. The radiographers and radiologists who worked with To-Be 1 have been blinded for study specific results during the study period. Only usual quality assurance has been performed and reported according to the guidelines.
To-Be 2
There are growing concerns about over-diagnosis and we should not take these lightly
Solveig Hofvind
The second part of the trial, To-Be 2, is a follow-up of the first analysis. All women who will attend the screening program in Bergen in 2018 and 2019 will be asked about participation and those agreeing will be screened with DBT and synthetic digital mammography. During the first 6 months, 93% agreed to participate. A certain number of the contributing women will have already participated in To-Be 1. ‘This means we can see the implications of using tomosynthesis after tomosynthesis, which will provide vital information. If we are to implement DBT in a screening program, we will use it every two years.
‘It is important to know if, for example, the increased detection rate still applies if we screen with tomosynthesis a second, third or sixth time,’ she explains. Within the first few months, the participation rate has already been over 93 percent. Just like To-Be 1, the second part of the trial will focus on performance, detection rate, as well as economical costs and consider interval cancers. Therefore the data will be ready for use in 2021. ‘We are expecting very interesting and relevant results from both parts of the trial,’ Hofvind believes. However, if the conclusions will further the process of including tomosynthesis in the Norwegian screening program remains to be seen. ‘We need more evidence to decide whether the technology really provides improvements. There are growing concerns about over-diagnosis and we should not take these lightly. If tomosynthesis is mostly detecting the small and slow-growing dormant tumours, we need to know and evaluate this fact, because after all,’ Hofvind emphasises. ‘Our goal in screening is to detect the killing cancers in time.'
Profile:
Professor Solveig Hofvind PhD heads the Norwegian breast cancer screening program, BreastScreen Norway, and is also a radiography lecturer at Oslo Metropolitan University. Having trained as a radiographer, she also obtained a master’s degree at the Norwegian school of sport sciences. Hofvind pioneered a breast clinic and the Norwegian breast cancer screening program at Akershus University hospital in Lørenskog, Norway, before she began to work for Norway’s cancer registry in 1998. Her PhD, granted in 2005, was gained for her thesis focused on the Norwegian breast cancer screening program.
10.07.2018