The impact of imaging on personalised cancer medicine
Enormous technical developments over recent decades, along with greater understanding of tumour biology, have made imaging, pathology and laboratory medicine indispensable tools in personalised cancer treatments.

Professor Hedvig Hricak, Chairperson of the Department of Radiology at Memorial Sloan-Kettering Cancer Center in New York, highlighted opportunities for advancing personalised cancer medicine through imaging at this year’s EFO, where EH Correspondent Bettina Döbereiner met up with her.
Professor Hricak prefers the word ‘precision’ to ‘personalised’, explained that in precision medicine, biomarkers are essential for precise diagnosis, therapy selection, therapy monitoring and early detection of recurrence. ‘To take a somewhat simplified view – three types of biomarkers are of special importance in cancer care: prognostic biomarkers for anticipating patient outcome regardless of the specific treatment, predictive biomarker for the outcome of treatment with a specific drug or other form of therapy, and early response biomarkers. Complementing the more widely accepted tools of pathology and laboratory medicine, imaging can provide important additions to the biomarker armamentarium.
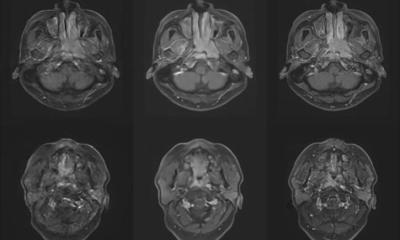
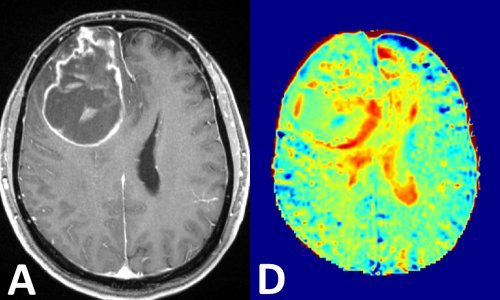
‘Perhaps the best way to explain the importance of imaging as a source of biomarkers is by giving an example: Consider a patient with breast cancer metastases in the brain. Today, for many targeted therapies we require biopsy before treatment selection, because we have learned that up to 30 percent of metastases de-differentiate— that is, have a different molecular profile than the primary tumour. Furthermore we have learned that there is tremendous heterogeneity in the genomic landscape of tumours, and that this heterogeneity can be found within and between tumour metastases in the same patient. It would be difficult to biopsy a single brain lesion, let alone obtain multiple biopsies from the same lesion or from different lesions in the same patient. Molecular imaging with different targeted tracers is the only answer for assessing the vast heterogeneity of cancer.’
Then it’s important in the selection of the right treatment?
‘Correct. It’s very important to know if metastases will respond to a treatment that targets the genetic signature of the primary tumour, or if they require different treatments. Imaging is indispensable for this purpose, especially when metastases are located in highly sensitive areas that are difficult to biopsy – such as the brain – or if there are more than two metastases, because it would be impossible to biopsy each one. We, and others in the field, have developed a number of novel radiopharmaceutical cancer specific tracers that can image a biology of a specific cancer metastasis – so we can now go beyond detection, which was the hallmark of anatomic imaging, to characterise the metastasis and thus choose the best treatment approach.
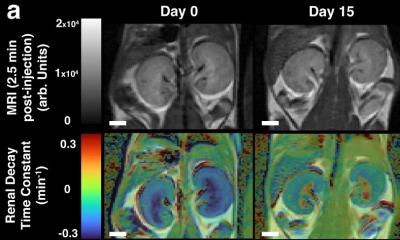
You mentioned that imaging biomarkers are also used to assess early response?
‘Yes, because sometimes, even if you’ve selected a certain drug based on the tumour’s specific characteristics, the tumour host reaction, that is to say the persondrug interaction may be different than expected. So, with molecular imaging, we can assess very early on if there is a response, or not.’
Where else is imaging in personalised medicine important?
‘It’s also very important for drug development, because we can use it to better select patients for clinical trials and obtain proof of principles sooner. For example, we performed a clinical trial for the new drug MDV3100, a form of androgen deprivation therapy, for metastatic prostate cancer. Theconventional follow-up CT scan showed no change. In the past, when we used CT findings as the measure of tumour response, we’d have thought that the therapy had failed. Adding the new molecular imaging technique of FDHT PET/ CT, an androgen receptor imaging, we saw a tremendous response following androgen deprivation therapy. So, to see the effects of targeted therapy, we need targeted imaging.
Is the FDHT tracer already on the market?
‘Unfortunately not; In my lecture I showed a list of 23 radiotracers that we have in clinical trials at MSKCC, and I don‘t know if you noticed, but the last column indicated that most of the tracers are being used under Memorial Sloan-Kettering Cancer Center FDA INDs for in-house use of those tracers. So we use a special FDA-approved mechanism to obtain permission for in-house use of those tracers. ‘Addressing regulatory requirements is a huge hurdle to widespread dissemination of new molecular imaging tracers. We need far more specific tracers than the commonly used tracer FDG, which shows only the metabolism of glucose. New radio-tracers can be specific for a common feature of tumour biology as in the case of FMISO, which evaluates hypoxia or specific for a certain kind of tumour as in the case of an androgen-receptor imaging for prostate cancer.’
Why aren’t these new radiotracers on the market?
‘It’s a regulatory problem: They still aren‘t FDA approved. I think today the regulatory approval and dissemination of molecular imaging agents are a bigger problem than the development of such agents. There is an urgent need to solve this problem and translate new radiotracers more rapidly to the clinical setting.’
10.07.2012