The future of radiology: Art or science?
Two things that radiologists resist – structured reporting and (computer-assisted) quantification – are the very things that Gabriel Krestin believes are essential to advance diagnosis in the brave new world of omic-medicine that is emerging.

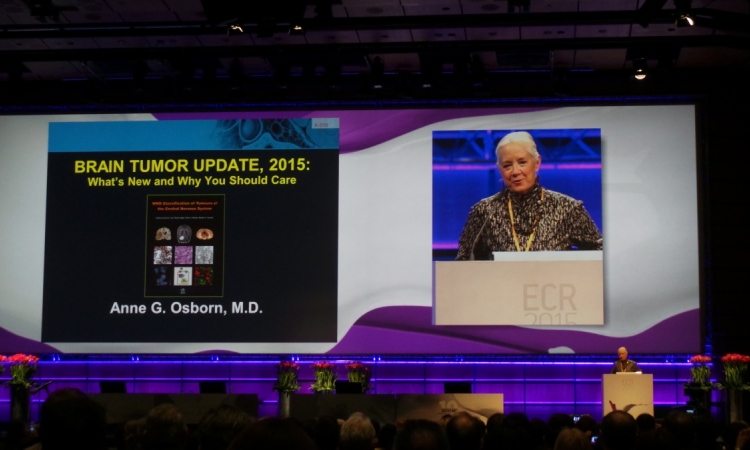
Thus, during the Sunday session Imaging In Precision Medicine, he will develop the subject in detail during an ECR 2014 presentation ‘Radiogenomics and personalised (precision) medicine’. Ahead of the congress, Professor Krestin spoke with European Hospital about the potential of linking genomic mutations with imaging phenotypes, the quantification of reporting it will require, and his views on changes necessary in both radiology and society.
EH: What is this new world of radiogenomics?
Gabriel Krestin: Radiogenomics has been used as a term in finding associations between the genetic signature, or genome, and certain imaging phenotypes, whether there are any imaging markers that are associated with genetic mutations. This is the term we, in radiology, usually use for this correlation between genomics and specific imaging signs. Imaging genomics is, more or less, the same definition and I think imaging genomics is the better term.
This is no longer a dream but a reality?
This is absolutely a reality. These types of studies have been exponentially increasing in recent years since the start of the Human Genome project. Now that we can increasingly sequence the whole genome in large numbers of cases and controls, people try to determine whether there is anything changed within a gene that is associated with a certain disease or a certain phenotype. Multiple cases have been found where such genes correlate or are associated with people who develop Alzheimer’s disease, or diabetes, Crohn’s disease or specific types of cancer or other chronic diseases.
The same techniques have been applied in large population studies. One of the first that we published, from Rotterdam, was whether there is a genetic mutation associated with white matter lesions in the brain. These lesions are a predictor for the development of cerebral vascular disease or Alzheimer’s disease. The question was whether there is a gene that predicts or is associated with white matter lesions. There is a potential for a lot more.
Where does radiology play a determining role in the universe of -omics?
A very exciting area that is not based on the overall genetic profile of the patient is leading to the genetic signature of a malignant lesion. This can become significant.
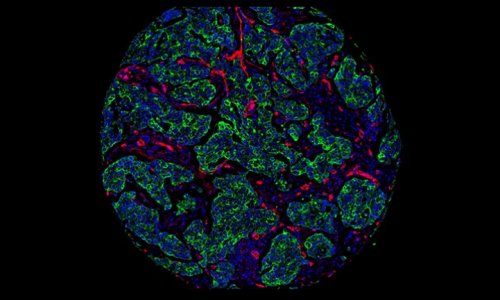
First, we can identify a certain number of patients with a certain type of cancer, biopsy that cancer, sequence the active genes that are expressed within that cancer type, and then correlate the genetic signature, the gene expression sequence, with hundreds of different imaging signs, like size, contours, the enhancement pattern, signal intensity on MR images and many other features that can be identified and characterised in a binomial way. Are the margins sharp or not sharp? You give it a 1 or a 0. Applying statistics, people have found very strong correlations between imaging features and the genetic signature of those tumours
It seems these imaging features may very well be a product of a certain genetic expression in that specific tumour – aggressiveness, for example. It seems there are certain genes that contribute to hypoxia in some tumours. We can find a correlation between that expressed gene and the enhancement pattern of that tumour. This will tell us if the tumour is hypoxic, or not. These are very relevant findings that have an implication on the possibilities to treat that tumour, because we know that tumours that are hypoxic will not respond to certain chemotherapies or radiotherapies.
Radiology has a 100-year tradition of interpreting images and reporting findings. Will this change that?
Absolutely. We are moving towards applying precision medicine in imaging. I’m absolutely convinced this is the way forward, and if we don’t want to be completely side-lined and made obsolete as radiologists, we have to move toward precision. Precision is measuring, structuring and standardising. I can understand that sometimes measuring and using these tools can seem quite boring. It’s much more rewarding to apply knowledge as an art instead of applying it as a science. I know how much resistance there is because it limits the freedom of professionals who are very much used to use their own words, to give descriptive findings.
Yet there is no way we can survive as a scientific specialty if we are only providing qualitative reports. We need to structure our reports. There are many activities in this area within the RSNA (Radiological Society of North America), within the ACR (American College of Radiology), and within the ESR (European Society of Radiology) – all pushing to adopt this concept of structured reporting.
In Europe it becomes more difficult because of the many languages, and it is difficult for diverse European societies to play a key role in adopting structured reporting. Yet, I believe there is no other way forward for the future.
Some radiologists also resist computer assistance for readings. . .
There is no way we can do this manually or even only based on visual interaction. Instead we develop imaging algorithms that do this work fully automatically. Processing image data with tools give us the numbers without any interaction between the reader and the images. We get brain volumes, the thickness of the cortex of the brain, or the volume of the white matter lesions, or the volume of the hippocampus.
Is there room still for art in radiology?
Good question. Hopefully there always will be and computers will never take over the integrative power of the brain. On the other hand, I’m very much in favour of standardisation. In a presentation on this topic I advocated that a patient, like someone taking a car to the garage, would like to know exactly what he would get for what he pays.
Today in a garage they work with lots of electronics tests to say what’s wrong with the car, and you immediately get an estimate to fix the problem. That is approximately what people would like in medicine, that you know what is going on, you know what to expect, you know what it will cost, and that, wherever you go, you will get the same type of care and cure without huge qualitative differences.
This is an ideal for the future. Yes, for many years there will continue to be differences, with better doctors than others, because so much is still not explained, and so much is still based on intuition and not purely on science.
Yet, the more we move toward finding the molecular basis of disease and the causes of disease, I hope we will move closer to the garage situation where you know exactly what you get, and whether it can be fixed or it can’t.
Who is going to pay for all this?
For the time being it’s interplay between the scientists and the organisations that are willing to fund these types of studies, such as national governments and European grants. Probably the pharmaceutical industry should be increasingly interested in this area because, through imaging genomics, they will get additional markers that can help in drug development.
Still, I have a different question. I never understood why the increasing cost of healthcare, in an industry that is growing much faster than other industries, is a problem. What’s bad about increasing the economy around healthcare? If 20% of a country’s population is employed in some way related to healthcare, why are we not willing to pay, or to allow that a significant part of the GDP goes into this industry? What is bad about that?
People want and need health. They are probably willing to pay for health, or the system should be willing to pay for health. I don’t see a huge problem. I have spoken with important economists about this and never received a good explanation as to why we want to limit the healthcare industry. We need a change in the mind-set.
Profile:
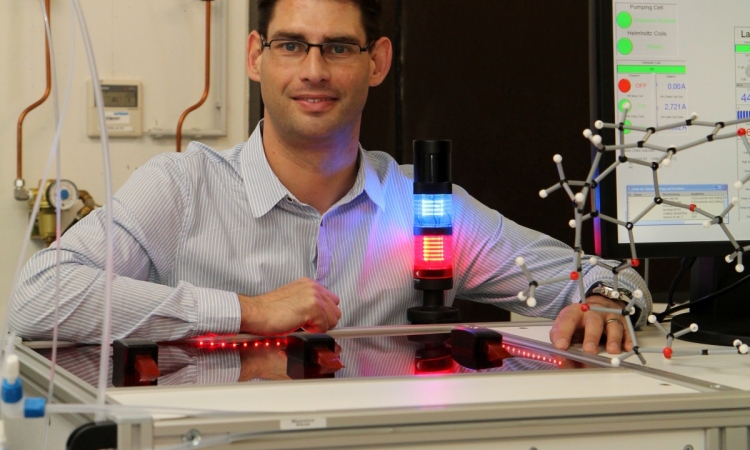
Professor of radiology and chairman of the radiology department at Erasmus University Medical Centre in Rotterdam, Gabriel Krestin is also the past-President of the European Society of Radiology and serves on the editorial and advisory boards of several journals, including European Radiology. He founded the working group Management in Radiology (MIR) and the European Institute of Biomedical Imaging Research (EIBIR).
07.03.2014