News • Obsessive compulsive disorder
Targeted deep brain stimulation reduces OCD symptoms
The debilitating behaviours and all-consuming thoughts which affect people with severe obsessive compulsive disorder (OCD), could be significantly improved with targeted deep brain stimulation, according to the findings of a new study.

OCD is characterised by unwanted intrusive thoughts (obsessions) and repetitive stereotyped behaviours (compulsions- sometimes called rituals) and often means everyday activities become impossible for those with the condition. This repetitive and compulsive behaviour is commonly associated with either depressed mood or impairment in cognitive flexibility – an inability to flexibly adapt to changing situations. Deep brain stimulation (DBS) is an emerging treatment for a small number of people with extremely severe OCD who have not responded to available treatment, such as cognitive behavioural therapy or medication. It requires neurosurgical implantation of electrodes.
In a study published in Biological Psychiatry, six patients with treatment-refractory OCD were recruited from NHS England Highly Specialised OCD Services. As part of the study, in a double-blind cross over trial, each patient received DBS stimulation to brain areas previously associated with OCD, the anteromedial subthalamic nucleus (amSTN) for three months and DBS stimulation to the ventral capsule/ventral striatal area (VC/VS) for three months, followed by DBS stimulation to both amSTN and VC/VS. The neurosurgery and clinical assessments were carried out at the Unit of Functional Neurosurgery and Hughlings Jackson Ward, The National Hospital for Neurology and Neurosurgery, Queen Square, London (part of UCLH).
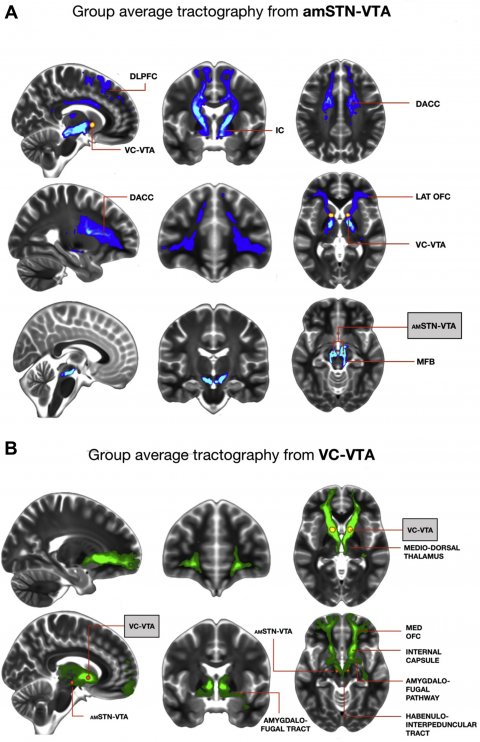
The study found that DBS at each site significantly and equivalently reduced OCD symptoms. However amSTN but not VC/VS DBS significantly improved cognitive flexibility, but VC/VS DBS had a greater positive effect on depressed mood. Furthermore, MRI tractography (a form of brain imaging) from optimally activated electrode contacts showed that the two DBS sites affected different neural circuits within the brain. This finding provides clues as to the roles that those specific brain regions play in OCD, and has potentially important implications for treatment.
Recommended article

News • Wireless WAND
Can 'pacemaker for the brain' help to treat neurological disorders?
A new neurostimulator developed by engineers at the University of California, Berkeley, can listen to and stimulate electric current in the brain at the same time, potentially delivering fine-tuned treatments to patients with diseases like epilepsy and Parkinson's. The device, named the WAND, works like a "pacemaker for the brain," monitoring the brain's electrical activity and…
DBS seems to offer a promising addition to treatments for those who have the most profound OCD which does not respond to all other treatments
Lynne Drummond
Lead author, Professor Eileen Joyce of University College London (UCL Queen Square Institute of Neurology), said: “This is the first study to compare directly the effects of deep brain stimulation at two brain sites and has discovered important information about how the brain changes in severe OCD responsible for obsessions and compulsions, depressed mood and cognitive inflexibility might be alleviated.”
Co-author Dr Lynne Drummond of St George's, University of London said: “All six of the patients showed marked improvements in their OCD symptoms with more than 35% reduction in symptoms. DBS seems to offer a promising addition to treatments for those who have the most profound OCD which does not respond to all other treatments. However we have not yet looked at long-term effects of this and more research will be needed to ensure that it continues to be effective.”
Cognitive flexibility was measured by the CANTAB IED test, and undertaken by researchers at Cambridge University. Their previous studies have shown that impaired cognitive flexibility is a marker of OCD and improvement implies that patients can break out of maladaptive routines and habits and take on new and rewarding experiences. All patients had been ill for at least 20 years and failed to respond to high doses of medication plus intensive CBT. Patients were recruited from NHS England Specialised OCD Services, at South West London and St George's Mental Health NHS and Hertfordshire NHS Partnership. Additional patient expertise was provided by the Advanced Interventions Service at the University of Dundee and NHS Tayside. The trials' first patient was recruited in 2013 and the sixth and final patient finished the study in November 2016. The study was by funded by grants from the MRC and Wellcome.
Source: St George's, University of London
03.04.2019