Image source: Scientific Animations (CC BY-SA 4.0)
News • Obsessive-compulsive disorder
Neural biomarkers for OCD discovered
For the first time, researchers at the Netherlands Institute for Neuroscience and Amsterdam UMC have identified what happens in neural networks deep within the brain during obsessive thoughts and compulsive behaviours.
Using electrodes implanted in the brain, they observed how specific brain waves became active. These brain waves serve as a biomarker for obsessive-compulsive disorder (OCD) and are an important step towards more targeted treatments.
The researchers published their findings in the journal Nature Mental Health.
OCD is a psychiatric disorder in which people suffer from obsessive thoughts (obsessions) and compulsive behaviours (compulsions). A well-known example is fear of contamination: someone is constantly afraid of becoming infected (the obsession) and feels compelled to wash their hands over and over again (the compulsion).
In psychiatry, it is almost never possible to link a symptom so directly to brain activity. This study shows that it is possible
Tara Arbab
In OCD, communication appears to be disrupted between the cerebral cortex, the striatum, and the thalamus, areas of the brain that together form the CSTC circuit. Normally, this circuit mainly coordinates movement and motivation.
For patients with particularly severe OCD, deep brain stimulation (DBS) is used as a treatment method. This involves placing electrodes deep in the brain to electrically stimulate parts of the CSTC circuit and thus reduce symptoms. While helpful in many cases, DBS does not fully or sufficiently alleviate symptoms in around 30% of the cases. Additionally, adjusting the stimulation to work effectively for a specific patient can sometimes take months.
To improve treatment, it is important to understand how disruption of the CSTC circuit is involved in OCD. Therefore, researchers from Ingo Willuhn’s group, in collaboration with colleagues from Amsterdam UMC, investigated what exactly happens in the brain during an obsessive thought and the subsequent compulsive action. This research, published today in Nature Mental Health, reveals important biomarkers for OCD. Prior to this publication, psychiatric symptoms could hardly be linked to brain activity with such temporal and anatomical precision.
In this study, the scientists used the implanted DBS electrodes to measure brain activity without stimulation. “We have been doing this in animal models for years,” says Tara Arbab, first author of the study, “but in patients, this technology is still new.” By better understanding what happens in the brain during obsessions and compulsions, researchers hope to increase the success of DBS.
During this study, patients were asked to consciously generate obsessive thoughts. For example, someone with a fear of contamination had to touch a dirty floor but was not allowed to wash their hands until later. Throughout this period, brain activity was measured in areas of the brain that are normally stimulated with DBS. “What makes this study unique is that we were able to measure deep brain activity with very high spatial and temporal precision,” says Arbab. “That’s not possible with an fMRI or EEG.”
The measured activity of entire neural networks was then filtered for brain waves with different frequencies. The researchers discovered that two of these waves, the alpha and delta waves, were particularly prominent during the performance of compulsive actions. These waves can therefore be specifically linked to OCD. ‘In psychiatry, it is almost never possible to link a symptom so directly to brain activity. This study shows that it is possible,’ says Arbab.
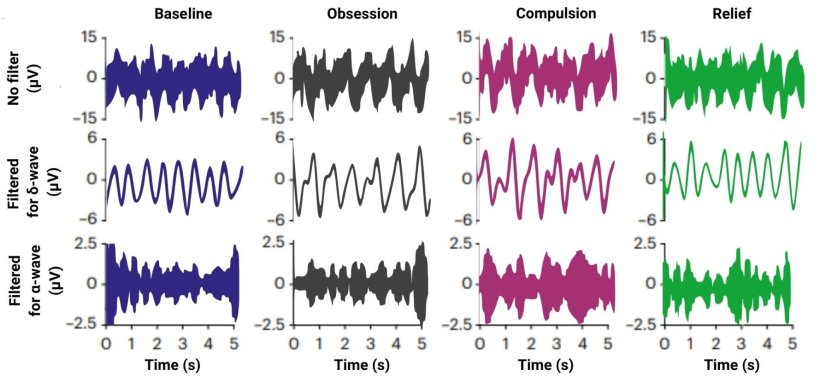
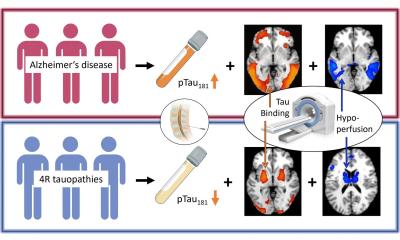
Image source: NIN-KNAW; adapted from: Arbab T, Bais MN, Figee M et al., Nature Mental Health 2025 (CC BY 4.0)
These findings bring science one step closer to a fundamental understanding of OCD. ‘For the first time, we have found a clear biological marker for OCD in the brain, a marker that we may be able to use in future treatments for OCD,’ says Arbab.
Currently, deep brain stimulation still works as a kind of “always on” system. The electrodes continuously emit electrical signals, without distinguishing between moments when this is necessary and when it is not. The newly discovered neural biomarkers therefore open the door to a smarter approach. ‘In the long term, we hope to switch to a system in which the electrodes only stimulate when they measure a signal that corresponds to compulsive behaviour,’ says Arbab. ‘That would make the treatment much more targeted.’
Source: Netherlands Institute for Neuroscience
26.07.2025