News • LDIR in neurology
The therapeutic potential of low-dose radiation for TBI and stroke
Traumatic brain injury (TBI) and ischemic stroke are major public health concerns and leading causes of death and disability worldwide.
Image credit: City University of Hong Kong
A research team led by City University of Hong Kong (CityU) neuroscientists recently discovered that low-dose ionizing radiation (LDIR), such as X-ray irradiation, can reduce lesion size and reverse motor deficits in TBI and ischemic stroke mice, demonstrating that LDIR may be a promising therapeutic strategy for TBI and stroke patients.
The findings were published in Brain, Behavior, and Immunity.
Nearly half of TBI and stroke survivors experience lifelong motor impairment and disability. “Usually, secondary brain damage worsens over time after primary injuries in TBI (mechanical insults such as a car accident or falls by older adults) and strokes (when blood flow to the brain is blocked), owing to the unfavorable and hostile neuroinflammatory environment in the brain,” explained Professor Eddie Ma Chi-him, in the Department of Neuroscience at CityU, who led the research. “But there is still no effective treatment for repairing the central nervous system after brain injury.”
It has long been known that low-dose X-ray irradiation can enhance adaptive responses, including extending average life expectancy, stimulating the immune system, healing wounds and stimulating cell growth in animals as well as neuroprotection in animal model of neurodegenerative diseases, primarily due to immunomodulation. Based on these studies, Professor Ma and his team speculated that the immunomodulatory effects of LDIR could play a pivotal role in mitigating damage and promoting wound healing after brain injury.
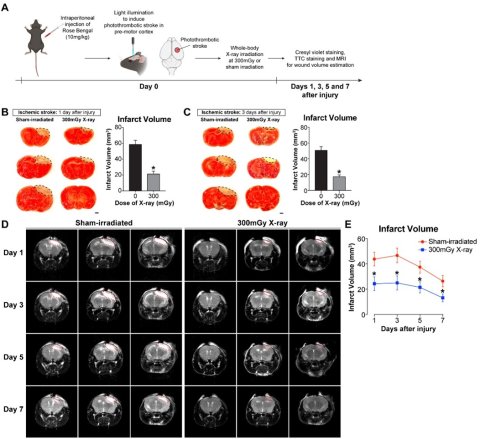
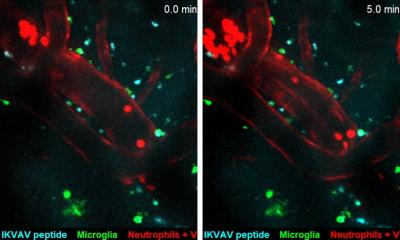
Image source: City University of Hong Kong; from: Au, N. P. et al., Brain, Behavior, and Immunity 2024
In their recent study, they found that low-dose X-ray irradiation completely reversed the motor deficits in TBI and stroke mice and restored brain activity after stroke. More importantly, low-dose X-ray irradiation treatment delayed by eight hours was still effective in allowing a complete recovery of motor function after stroke, which is highly clinically relevant in the translation of the findings into clinical applications, since this is very likely to happen in the clinical setting, where hours could elapse before any treatment is available.
Mice were treated with whole-body X-ray irradiation after cortical stab wound injury or photothrombotic ischemic stroke, while the control mouse group received no (sham) irradiation. Seven days after cortical stab wound injury, the X-ray-irradiated mice exhibited a reduction in lesion size by 48%. The magnetic resonance imaging showed that X-ray irradiation significantly reduced the infarct volume of stroke mice by 43–51% during the first week after the induction of ischemic stroke. These results support a common clinical observation that stroke patients with smaller infarct volume usually have improved clinical outcomes.
Moreover, X-ray irradiation accelerated substantial motor function recovery detected by narrow bean walking, pole climbing and grip strength after cortical stab wound injury and ischemic stroke. For instance, X-ray-irradiated mice took a much shorter time to transverse a narrow beam, with fewer foot slips, indicating that X-ray-irradiated mice demonstrated excellent motor coordination and balance shortly after cortical stab wound injury and ischemic stroke.
We believe this strategy could be used to address unmet medical needs in accelerating motor function restoration within a limited therapeutic window after severe brain injury, like TBI and stroke
Eddie Ma Chi-him
The team also conducted systems-level transcriptomic analysis, which showed that genes upregulated in LDIR-treated stoke mice were enriched in pathways associated with inflammatory and immune responses involving microglia. LDIR induced upregulation of anti-inflammatory- and phagocytosis-related genes, and downregulation of key pro-inflammatory cytokine production. This suggests that LDIR treatment has a strong immunomodulatory effect by the expression of genes involved in inflammatory and immune responses.
More strikingly, their study demonstrated that the LDIR promoted axonal projections (brain rewiring) in the motor cortex and recovery of brain activity detected by electroencephalography recordings months after stroke. Even if the LDIR treatment was delayed by eight hours after the injury, it still maintained the full therapeutic effect on motor recovery.
“Our findings indicate that LDIR is a promising therapeutic strategy for TBI and stroke patients,” said Professor Ma. “X-ray irradiation equipment for medical use is commonly available in all major hospitals. We believe this strategy could be used to address unmet medical needs in accelerating motor function restoration within a limited therapeutic window after severe brain injury, like TBI and stroke, warranting further clinical studies for a potential treatment strategy for patients.”
The first author is Dr Au Ngan-pan, a CityU PhD graduate and currently a lecturer at the University of Portsmouth. The corresponding author is Professor Ma. Other CityU collaborators include Professor Kannie Chan Wai-yan and Professor Peter Yu Kwan-ngok, and PhD students Wu Tan and Joseph Lai Ho-chi. The research was supported by the General Research Fund of the Research Grants Council, the Health and Medical Research Fund of the Food and Health Bureau of the Hong Kong SAR Government, and the Shenzhen Science, Technology and Innovation Commission.
Source: City University of Hong Kong
30.01.2024