Brain Injury and Disease
Researchers Identify How Inflammation Spreads Through the Brain After Injury
Researchers have identified a new mechanism by which inflammation can spread throughout the brain after injury. This mechanism may explain the widespread and long-lasting inflammation that occurs after traumatic brain injury, and may play a role in other neurodegenerative diseases.
The findings were published today in a study in the Journal of Neuroinflammation.
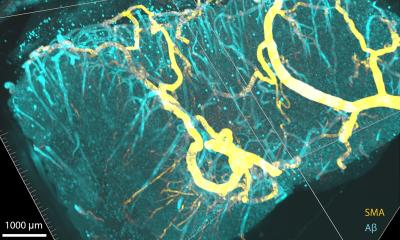
This new understanding has the potential to transform how brain inflammation is understood, and, ultimately, how it is treated. The researchers showed that microparticles derived from brain inflammatory cells are markedly increased in both the brain and the blood following experimental traumatic brain injury (TBI). These microparticles carry pro-inflammatory factors that can activate normal immune cells, making them potentially toxic to brain neurons. Injecting such microparticles into the brains of uninjured animals creates progressive inflammation at both the injection site and eventually in more distant sites.
Research has found that neuroinflammation often goes on for years after TBI, causing chronic brain damage. The researchers say that the microparticles may play a key role in this process.
Chronic inflammation has been increasingly implicated in the progressive cell loss and neurological changes that occur after TBI. These inflammatory microparticles may be a key mechanism for chronic, progressive brain inflammation and may represent a new target for treating brain injury.
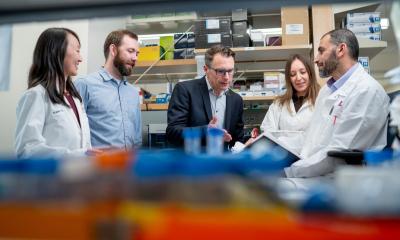
The researchers on the paper include four University of Maryland School of Medicine researchers: Alan Faden, Stephen R. Thom, Bogdan A. Stoica, and David Loane.
“These results potentially provide a new conceptual framework for understanding brain inflammation and its relationship to brain cell loss and neurological deficits after head injury, and may be relevant for other neurodegenerative disorders such as Alzheimer disease in which neuroinflammation may also play a role,” said Dr. Faden. “The idea that brain inflammation can trigger more inflammation at a distance through the release of microparticles may offer novel treatment targets for a number of important brain diseases.”
The researchers studied mice, and found that in animals who had a traumatic brain injury, levels of microparticles in the blood were much higher. Because each kind of cell in the body has a distinct fingerprint, the researchers could track exactly where the microparticles came from. The microparticles they looked at in this study are released from cells known as microglia, immune cells that are common in the brain. After an injury, these cells often go into overdrive in an attempt to fix the injury. But this outsized response can change protective inflammatory responses to chronic destructive ones.
The findings have important potential clinical implications. The researchers say that microparticles in the blood have the potential to be used as a biomarker – a way to determine how serious a brain injury may be. This could help guide treatment of the injuries, whose severity is often difficult to gauge.
They also found that exposing the inflammatory microparticles to a compound called PEG-TB could neutralize them. This opens up the possibility of using that compound or others to treat TBI, and perhaps even other neurodegenerative diseases.
Source: newswise
09.03.2017