Article • Cancer diagnostics
Progressing towards optical biopsy
Recognising malignant tissue remains a tricky task. While today, most patients undergo a biopsy, an invasive procedure where tissue is sampled, stained and assessed, researchers are exploring the potential of optical biopsy, the visual assessment of suspect tissue.
Report: Sascha Keutel
Simply put, in optical biopsy a light beam is directed towards the suspect tissue and the optical response is recorded
Thomas Bocklitz
The interest in optical biopsy ‘is indeed enormous,’ confirms Dr Thomas Bocklitz, physicist at Friedrich-Schiller University in Jena, Germany. The physicist heads the joint working group ‘Statistical modelling and image analysis’ at the Leibniz Institute for Photonic Technology and Friedrich-Schiller University Jena, which looks at different aspects of optical biopsy. ‘Simply put,’ Bocklitz explains, ‘in optical biopsy a light beam is directed towards the suspect tissue and the optical response is recorded. ‘In a second step, diagnostic parameters are deducted from this response. In other words, we replace the removal of suspect tissues by direct, in-situ measurement.’
A non-invasive and quick procedure
Optical biopsy offers several advantages compared to conventional biopsy – take, for example, ENT frozen section: in a conventional procedure the patient undergoes surgery under general anaesthetic. The surgeon removes the tumour tissue and takes samples from the tissue margins, which are sent to the pathologist. It can take up to 40 minutes for results to reach the operating theatre (OT) since not every hospital has an in-house lab. If the pathologist detected tumour cells in the margin samples, the surgeon has to remove further tissue, take another sample and send it to the lab again. This cycle is repeated until the sample is tumour cell-free.
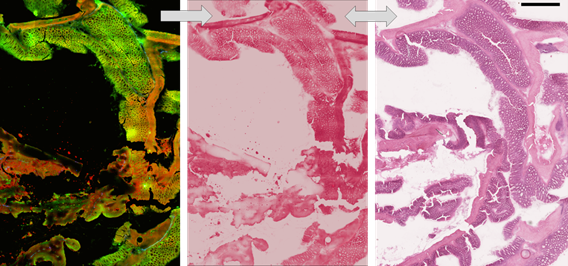
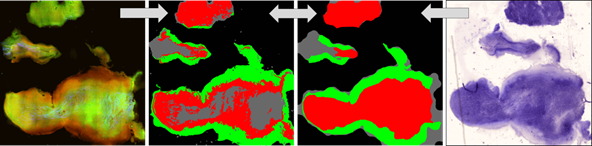
‘Optical biopsy, however, is performed by a technical assistant at the OT table. The acquired optical images are digitally stained. The results are forwarded to the pathologist – a procedure which saves time and is less strenuous for the patient. Moreover, the optical images contain additional information which can be used beyond sample staining,’ explains Bocklitz. This is just the beginning – researchers are already thinking one step further: they want to implement the measurement directly via fibres and have an endoscopy specialist, or surgeon, assess the results directly. ‘The surgeon places the fibres on the tissue and can tell right away whether the tissue contains tumour cells. If yes, he can adjust the tissue mass to be removed. This would mean that really only cancer tissue is removed – healthy tissue will be spared.’
Multi-modal imaging en-ables digital image analysis of tissue samples

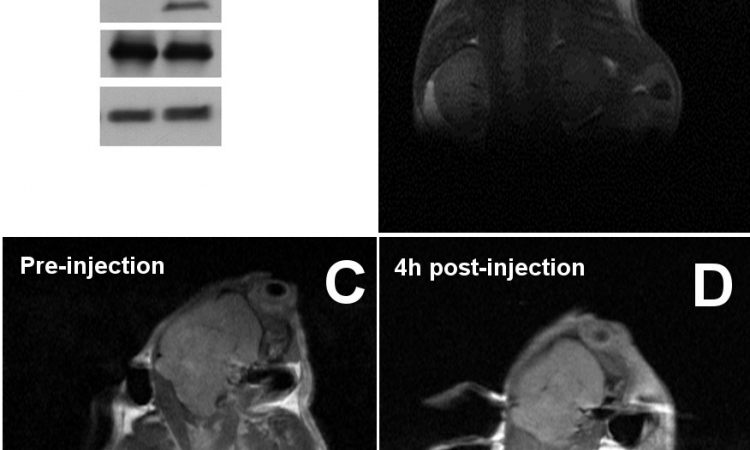
The crucial step in optical biopsies is processing the optical images – the focus of Bocklitz’s work. He not only developed the above conversion of optical images into digital stains but also a classification model. This model, a cooperation project with the ENT clinic at University Hospital Jena, offers automated tissue assessment based on images acquired ex-vivo or in-vivo.
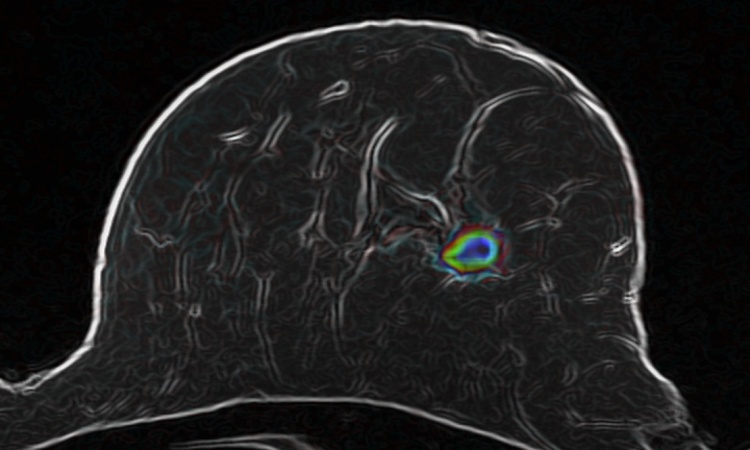
The imaging methods Bocklitz and team use combine several optical techniques. ‘We simultaneously acquire several types of multi-modal images: coherent anti-stokes Raman scattering, second harmonic generation and two-photon excited auto-fluorescence. These three mechanisms visualise the distribution of lipids and proteins as well as the distribution of the tissue’s fluorophores and fibre structures. ‘We developed an analysis of these multi-modal images for automated delineation of cancer and healthy tissue as well as algorithms that cull quantitative clinical information from the measuring data,’ Bocklitz explains. His message: ‘This is radiomics for pathologists!’
We take certain features of the image that quantify morphologies or textures and extract those values. Then we apply standard classifiers to differentiate healthy from pathological epithelial tissue
Thomas Bocklitz
When developing these image analysis algorithms the researchers tried to transfer the standard procedure pathologists use – haematoxylin and eosin staining – to the computer. The pathologist looks at the section and assesses tissue structure and morphology. ‘We can teach the computer to recognise patterns,’’ Bocklitz explains. ‘We take certain features of the image that quantify morphologies or textures and extract those values. Then we apply standard classifiers to differentiate healthy from pathological epithelial tissue. These classifiers are used to calculate the significant differences between the two groups and to predict the difference.’ Pattern recognition is the alpha and omega – the acquired skill that allows the computer to tell clear cases from unclear ones and thus reduce the pathologist’s workload.
In an initial study, involving ten patients, the accuracy rate of the diagnoses was 90 percent. A multi-centre pre-clinical study is currently being designed to analyse several hundred cases. By increasing the number of patients, Bocklitz hopes to increase accuracy to over 95 percent. Moreover, in this upcoming study the team will perform the measurement in a lab right next to the OT, to be able to integrate optical biopsy into the surgery workflow.

Bocklitz considers the preliminary results of optical biopsy to be very promising. The data that were generated optically contain a lot of information that will improve patient care. ‘Initially, there will be a combination of different measuring methods. Each method provides different data, which we will be able to pool. However, this scenario requires the development of suitable and high-performing algorithms for assessment, because we have created a multidimensional data space that needs to be analysed.’ In the long run, Bocklitz predicts, ‘optical biopsy will surpass conventional biopsy in terms of accuracy and information value.’
Profile:
PD Dr Thomas Bocklitz studied physics at the Friedrich-Schiller-University in Jena, Germany. He received his diploma in theoretical physics in 2007 and PhD in chemometrics in 2011. Today he heads a junior research group for statistical modelling and image analysis. His research agenda is closely connected with the translation of physical information, measured by Raman-spectroscopy, AFM, TERS, CARS, SHG, TPEF, into bio-medical biological relevant information. This research has led to over 80 reviewed publications and his habilitation. In 2015 he was awarded the Bruce-Kowalski Award for chemometrics and, in 2016, the Beutenberg-Campus Jena e. V. Science Award.
05.03.2018