Article • Keynote on integrated diagnostics
Predicting – and shaping – the future of modern pathology
Complex diseases could require complex biomarkers for accurate diagnosis in the years ahead, according to a leading pathologist. In a keynote address to the 36th European Congress of Pathology in Florence, Italy, Professor Manuel Salto-Tellez highlighted this as one of the major future challenges for the discipline. However, he also believes pathologists will sit at the core of modern medicine.
Report: Mark Nicholls

As he opened his address, the Professor of Integrative Pathology at the Institute of Cancer Research in London (ICR) and Professor of Molecular Pathology at Queen’s University Belfast (QUB) reflected on the last two decades looking in pathology and how at the turn of the millennium, he suspected few would have been able to predict the advances, and the speed at which they have been made, in the intervening years.
In his presentation, Salto-Tellez also referred to the challenge in 1999 from Dr Harold Vamus, Director of the US National Institute of Health, for the scientific community to change the basis of tumour classification ‘from morphological to molecular characteristics.’ Despite the pessimism it created then about the future of the discipline, he said: ‘Could we have predicted that 25 years later, there were more samples than ever coming into pathology departments with an increase of 5% per year and that many of the predictive markers we used in personalised medicine are actually driven by good old immunohistochemistry?’
Disease vs biomarker complexity: levelling the playing field
‘So, how do we start predicting the future?’ asked Salto-Tellez. While there are new drugs, clinical trials and technologies, he focused on new biomarkers as pivotal in translating discovery into applicability and prediction of treatment response.
Focusing on immuno-oncology (IO) and advances in pathology, particularly with the advent of artificial intelligence (AI), he discussed the complex biology of the tumour microenvironment, the complex biomarkers and what pathologists can offer today in IO diagnostics with PD-L1, microsatellite instability, tumour mutational burden, and – in the boundary between clinical trials and diagnostics – the analysis of T-cell response and tumour infiltrating lymphocytes (TILS). ‘We are dealing with complex disease with very simple biomarkers,’ he said. ‘But it could be that complex disease need complex biomarkers. To me, this is going to be that challenge that we are going to see over the next few years.’
Advancing that can mean extracting the complexity that exists in images; harnessing new technologies; or better use of information available in hospitals and ‘begin to integrate that in new algorithms that are hopefully going to better help our patients.’
The future is digital
He pointed to studies in digital pathology and AI that ‘tell us that a pathology service that is digitised is better. But this is only the beginning because we know that the in-silico image is going to allow us to extract significant information for the future.’
Such tools, however, need to be intuitive to use, meaningful for the pathologist and scientist, quantitative, and correlate with clinical outcomes. The AI architecture, with numerous tools now available to pathologists, can be used to identify histological features better, predict molecular biomarkers and quantitate single and multiple biomarkers.
Recommended article

Article • In-depth
Focus on digital pathology
Digital pathology opens up a whole new world of possibilities in diagnosis, prognosis, and prediction of diseases. Keep up-to-date with the latest research news, medical applications, and background information on digital pathology.
New methods against PD-L1 ‘madness’
Prof Salto-Tellez also reflected on the current complex pathology pathway in the realms of molecular diagnostics. ‘It is fragmented and as pathologists, we probably need to start thinking about how we rationalise this.’ He expanded on this by referring to the ‘madness’ with PD-L1, where pathologists are dealing with multiple scoring systems associated with individual drugs, antibodies and auto-stainers which have to be scored and defined differently, depending on the cancer type.
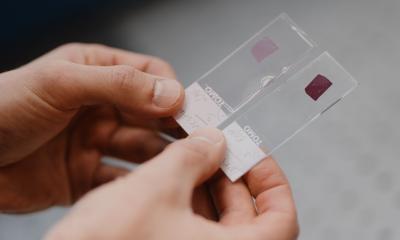
His QUB team is working to create prototypes to match the H&E and PD-L1 staining to mark the area of tumour and then render a potential result. When translated into an AI in a system together with other potential prognosticators, he said that can begin to tell the prognosis of individual patients. ‘Through the tools we have today, we are beginning to generate new complexity,’ he said.
Medical information talks – if we let it
Further ICR work, he said, has examined tens of clinical trials and is using tools to identify every potential member of the tumour microenvironment. ‘An important component of what we do in the future is associated with clinical trials, but until now clinical trials have been the lost opportunity to develop biomarkers meaningfully,’ he suggested. ‘The trend we see is that we probably apply AI too late in the process. It may make sense to bring this forward and start generating AI tests up front.’
A critical step in delivering integrative diagnostics into hospital settings and generate new algorithms to help patients involves accessing information in real life in the hospitals, the expert pointed out. ‘The reason we are not able to extract information for patients immediately and start applying these tools is because that information is in siloes – lab information management systems (LIMS), electronic health records (EHR), other records, images, are not talking to each other. That is the main bottleneck.’
‘Custodians of multiplex diagnostic opinion’
A survey of clinicians suggested genomics, histopathology, digital pathology tools, AI results, radiology and radiomics, EHR and LIMS should be integrated. However, three main questions must be answered to overcome this challenge, Salto-Tellez said:
- are we ready in our hospital to manage that information in that way?
- do we have computation technology to create that integration?
- how can accreditation be brought to a test that is an amalgamation of different systems?
‘This is important because to me, the main custodian of that multiplex diagnostic opinion should be the pathologist,’ said Salto-Tellez. ‘We should be the ones leading this opinion. My prediction is that we are looking at a fourth revolution: how to integrate our resources and how we bring that information into our patients is going to dictate the future.’
Profile:
Manuel Salto-Tellez is Professor of Integrative Pathology at the Institute for Cancer Research in London (ICR), and the lead of the Royal Marsden Hospital/ICR Integrated Pathology Unit. He is also the Chair of Molecular Pathology at Queen’s University Belfast (QUB), a clinical consultant pathologist and the Lead of QUB’s Precision Medicine Centre of Excellence, and author or co-author of more than 320 internationally peer-reviewed articles in translational science, molecular pathology and diagnostics.
02.01.2025