Pneumonia research in Spain
In November 2009 about 150 leading infectious disease researchers gathered in Berlin for the National Forum for Innovation in Medicine. During the meeting, Professor Antoni Torres MD (Hospital Clinic-Ciberes, University of Barcelona) gave Meike Lerner insights into community acquired pneumonia research projects and findings

In the international medical community, Prof. Antoni Torres is internationally deemed to be a physician of reference both nationally and internationally in lung infections -- including pneumonia, chronic obstructive pulmonary disease (COPD), bronchiectasis, immunocompromised patients, weaning, non-invasive ventilation (NIV), and acute respiratory distress syndrome (ARDS-ALI).
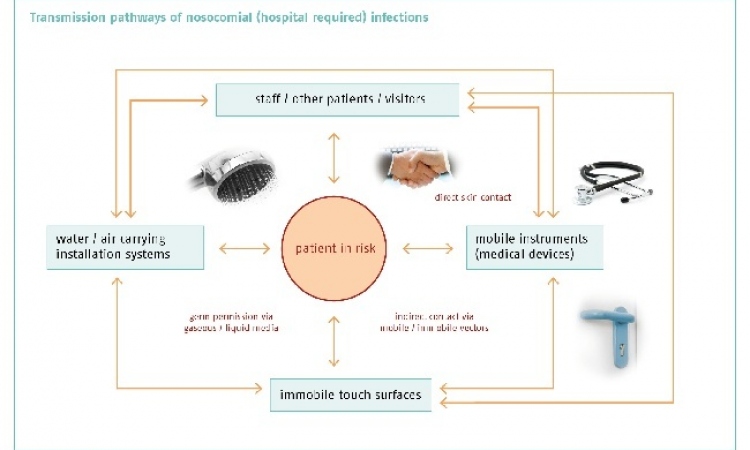
His Barcelona team mainly investigates community-acquired and intra-hospital respiratory infections, aiming to answer questions arising from clinical observation of patients that are not in the literature and to obtain results that can be quickly applied to diagnosis, treatment and prevention of nosocomial pneumonia. Additionally, in their community-acquired respiratory infections studies they approach important questions e.g. decisions regarding hospital or intensive care unit (ICU) admissions, microbial aetiology, diagnostic tests and best treatments.
‘We have been investigating community-acquired and hospital-acquired pneumonia for several years. We have a network in Spain that prospectively collects -- from several hospitals -- consecutive community-acquired pneumonia cases admitted to hospital and not admitted to hospital. We know that the incidence of community-acquired pneumonia ranges between two and eight cases per 1,000 inhabitants per year. This incidence increases with age, where we even talk about 65 cases per 1,000 in hospital inhabitants per year. And, as the elderly population increases so does the number of community-acquired cases and the number of ICU admissions.
‘Approximately, 40-60% of community-acquired pneumonia patients need hospital admission. So this is a very important burden. For example, in the hospital clinic in Barcelona, we admit about 500 patients per year -- a lot for a hospital with 750 beds.
‘Another increasing problem in the community is the so-called healthcare associated pneumonia (HCAP). Some patients outside of the hospital are admitted into nursing home care, or they have risk factors for a different type of pneumonia, for example, administration of medication intravenously, or immunosuppression, dialysis, or other factors associated with healthcare beyond the hospital. When these patients have pneumonia they are sicker, they may have different aetiology compared with patients with simple community-acquired pneumonia and probably need different treatment. Since that population is increasing, we have more and more patients now in nursing healthcare facilities.
‘This is an important issue in terms of the burden and the cost of pneumonia beyond the hospital. For these two types of pneumonia -- community-acquired and HCAP -- we have moved the centre projects here in Spain to study the aetiology, resistance of microorganisms and the treatment response and how to monitor it.
‘An important issue that has been recognised in the last year is the inflammatory response of these patients to pneumonia and potential mobilisation of the inflammatory response. We have another network in 13 Spanish hospitals that is studying the problem of healthcare-associated pneumonia and we hope that we will have some important results by the end of the year, particularly regarding the micro-aetiology of that population.’
‘The right treatment -- in medical terms adequacy -- is a very important issue. Adequacy means that we are giving an antibiotic that covers a specific micro-organism that is not resistant to it. The initial treatment is related to lowered mortality, which is very important. For community-acquired pneumonia, the right treatments have been released and published in different guidelines, for example, the European Respiratory Society guidelines published in 2005, or even the ATS/IDS published in 2007. So, they have sped up some recommendations in these guidelines, but they are easy to follow and if the physicians follow these recommendations adequacy is guaranteed, which has beneficial consequences in mortality.
‘As for the future, we believe that the important findings -- for example in the prevention of hospital-acquired infections and hospital-acquired pneumonia -- must first be tested in animals. For that purpose, we have developed an animal model of hospital-acquired pneumonia in piglets, which we intubate and ventilate, and we perform studies on the pigs to determine strategies of prevention and treatment. We want to support and potentiate these models. For example, we have studied the use of corticosteroids as an adjunctive therapy, in very similar pneumonia cases, to decrease the inflammatory response. We published these results very recently. Now we are doing more experiments in the piglet model. For example, studying strategies aimed to decrease the aspiration of pharyngeal contents to the lower airways, which is one of the mechanisms related to the development of pneumonia. We also want to study new molecules to mobilise inflammation. Our models are caused by Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus -- the two main micro-organisms involved in hospital-acquired pneumonia.’
26.01.2010