News • Polycystic ovary syndrome
PCOS: discovery of four subgroups enables personalized treatment
Four distinct subgroups of polycystic ovary syndrome (PCOS) have been identified in an international study by researchers from Karolinska Institutet, among others.
The results, published in the journal Nature Medicine, open up for more tailored treatments for the millions of women living with the disease worldwide.
PCOS is a common hormonal disorder that affects the function of the ovaries and affects approximately 11-13% of women of childbearing age. In the current study, the researchers analyzed clinical data from over 11,900 affected women over a period of 6.5 years. The results were confirmed in five international cohorts from Asia, Europe, and the US.
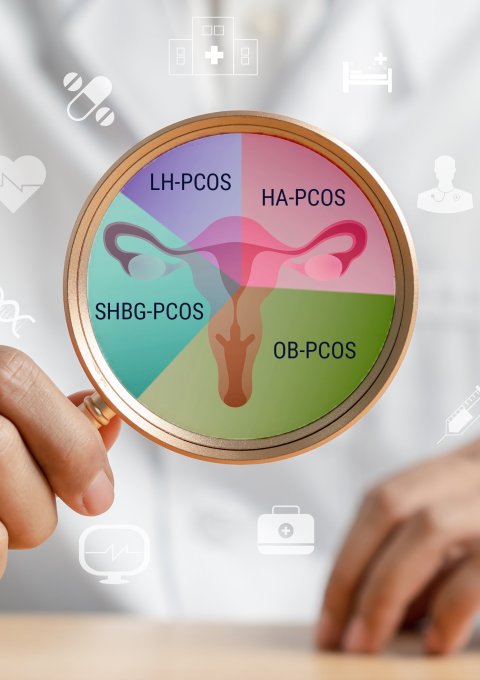
© Kiattisak – stock.adobe.com; data from: Gao X, Zhao S, Du Y et al., Nature Medicine 2025
Four PCOS subgroups were identified based on clinical measurements:
- HA-PCOS (Hyperandrogenic phenotype): Characterized by elevated levels of male sex hormones. This group had the highest risk of miscarriage in the second trimester and the highest incidence of abnormal blood lipids.
- OB-PCOS (Overweight-obesity phenotype): With higher BMI and insulin resistance, this group exhibited the most pronounced metabolic problems, the lowest proportion of live births, but also the highest proportion who recovered from PCOS over time.
- SHBG-PCOS (High level of sex hormone-binding globulin): A milder form of PCOS with fewer fertility problems and the lowest risk of diabetes and high blood pressure.
- LH-PCOS (Elevated luteinizing hormone and antimüllerian hormone, AMH): This group had the highest risk of ovarian hyperstimulation syndrome (OHSS) during IVF and the lowest rate of recovery.

Image source: Karolinska Institutet; photo: Anneli Nygårds
The results show clear differences in pregnancy rates, live births, and complications between the subgroups.
“Women with SHBG-PCOS had the best IVF outcomes, while OB-PCOS and HA-PCOS were associated with more miscarriages and metabolic complications such as abnormal blood lipids and type 2 diabetes,” says Elisabet Stener-Victorin, professor of reproductive physiology at the Department of Physiology and Pharmacology, Karolinska Institutet and one of the study's leaders.
The study also shows that different IVF strategies may work better for certain PCOS subgroups. ”For example, women with HA-PCOS responded better to the transfer of frozen embryos compared to the transfer of fresh embryos – a finding that may influence future treatment practices,” says Elisabet Stener-Victorin.
The researchers now hope that the results will pave the way for a new type of personalized care. “By identifying subgroups within PCOS, it is possible to start applying precision medicine, where care can be tailored to each woman's unique risk profile,” says Elisabet Stener-Victorin.
As part of the project, the researchers have developed a web-based tool, PcosX, which makes it possible to classify patients into subgroups based on nine standardised clinical measurements. "This international collaboration has provided robust evidence that could change how we diagnose, treat, and follow up on women with PCOS. It also emphasises that treatment can be tailored to the PCOS subtype to better capture the biological variation in PCOS,“ says Elisabet Stener-Victorin.
Source: Karolinska Institutet
31.10.2025





