Article • Finding therapeutic targets
Pancreatic cancer: Seeking viable treatment strategies
Pancreatic cancer has the worst survival rate of any cancers, with immunotherapies currently offering negligible treatment benefits for patients. To help identify new therapeutic approaches, researchers from the University of Oxford have been focusing on leukocyte infiltration as a prognostic marker of the disease.
Report: Mark Nicholls

Their study and findings were outlined by Dr Shivan Sivakumar during a session that discussed the latest developments in immunology and immunotherapy at the National Cancer Research Institute (NCRI) Virtual Showcase, held online on 2/3 November.
In opening his presentation ‘Immune responses in pancreatic cancer may be restricted by prevalence of activated regulatory T-cells, dysfunctional and senescent T-cells’, Sivakumar pointed out that pancreatic cancer has a five-year survival of 7%, with 20% survival with early diagnosis. The outlook is often bleak for patients with advanced disease and chemotherapy remains the mainstay of treatment. ‘We know the last few years has been a real revelation in therapeutics with immunotherapy, which has changed the paradigm in several cancers and demonstrated response rates in most cancers’, Sivakumar said. ‘Unfortunately, in pancreatic cancer, the two main classes of checkpoint inhibitors: anti-PD 1 and anti-CTLA4 – T-cell therapy - have demonstrated no survival benefit. From work done by ourselves and others, we know that T-cells exist within pancreatic cancer, so this led us to ask the questions: What are the T-cell phenotypes within pancreatic cancer? What are their activation and exhaustion statuses? and Are there other the novel strategies we can employ?’
Recommended article

Article • Cystic lesions of the pancreas
A more complex question than ‘good’ vs ‘bad’
Cystic lesions of the pancreas can occur in many forms, not all of which pose a serious threat to the patient. A thorough diagnosis using multi-modality imaging is therefore indispensable to differentiate between benign and malignant lesions.
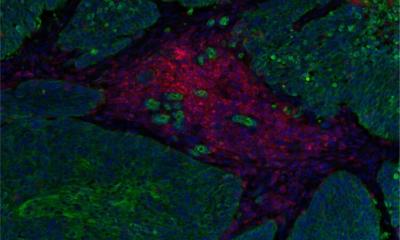
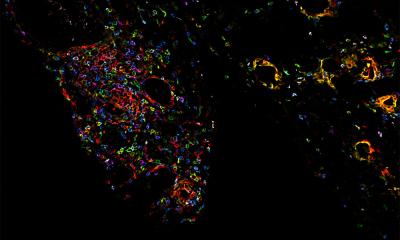
Dr Sivakumar, an academic medical oncology consultant at Oxford University, explained that, for this research, a T-cell focused CyTOF panel was used to analyse 32,000 T-cells from eight pancreatic cancer patients. This enabled them to describe the proportions of the three main compartments within pancreatic cancer; the stroma, fibroblast immune, and cancer panel.
Whilst their findings were consistent with the literature – that most cells within these tumours are fibroblasts – they found a significant immune component within these tumours. Looking at T-cell phenotypes, they hypothesised that the lack of activity of inhibitors indicated that there were probably no prominent PD-1 immune pathways in pancreatic cancers, so they tested this by re-evaluating T-cell states unto their microenvironment and analysed T-cell functions.
Our work identifies novel therapeutic targets that should form the basis for rational design of a new generation of clinical trials
Shivan Sivakumar
A striking observation was that these cells displayed senescent characteristics, whilst maintaining their cytolytic capabilities. This, he added, is the first time they have been reported within pancreatic cancer. Further T-cell investigation demonstrated the majority of CD8 T-cells have intermediate to low PD1 expression suggesting why PD1 may not work as a pancreatic cancer therapy strategy. The findings indicate that T-reg cells are major players in the suppressive microenvironment of pancreatic cancer, contributing to its poor prognosis. ‘Our work identifies novel therapeutic targets that should form the basis for rational design of a new generation of clinical trials,’ Sivakumar surmised.
The study concluded that, for future immunotherapy studies in pancreatic cancer, inhibition of TIGIT (an immune receptor of T-cells) or ICOS (a T-cell co-stimulator) may be a more viable treatment strategy than PD1. He pointed out that anti-TIGIT and anti-ICOS trials are ongoing.
Other presentations in the session on immunology and immunotherapy included a focus on how RAS orchestrates the increase of interstitial adenosine in lung adenocarcinoma to promote immune evasion and how radiation and DMXAA limit tumour development in a urethane-induced lung cancer model through inflammatory response.
Profile:
Dr Shivan Sivakumar is an academic medical oncology consultant and a clinical career development fellow in the Department of Oncology at the University of Oxford, with an interest in experimental pancreatic cancer medicine and in developing novel therapeutic strategies for this recalcitrant disease. He also sees patients in a dedicated HPB (Hepatopancreatobiliary) research clinic where patients are recruited for dedicated translational studies.
19.11.2020