Article • Cystic lesions of the pancreas
A more complex question than ‘good’ vs ‘bad’
Cystic lesions of the pancreas can occur in many forms, not all of which pose a serious threat to the patient. A thorough diagnosis using multi-modality imaging is therefore indispensable to differentiate between benign and malignant lesions.
We spoke with Professor Valérie Vilgrain, from Hôpital Beaujon, Hôpitaux Paris-Nord Val de Seine, in Clichy, France, about the prevalence of cystic pancreatic lesions and the right imaging tools to establish a reliable diagnosis.
What are cystic lesions?

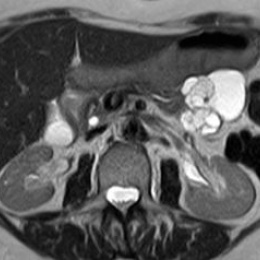
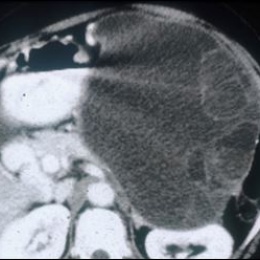
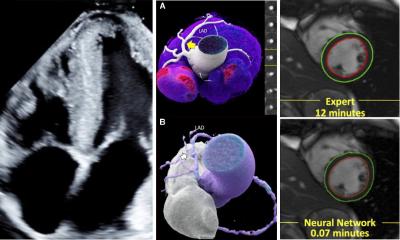
Pancreatic cystic lesions are very heterogeneous and extremely common. Interestingly, their recorded prevalence is directly related to the imaging modality used for their detection. While prevalence on CT-scan is 2-3%, on MR it ranges between 13-45%. This is an especially important finding because, more often than not, the MRI would have been prescribed to examine an unrelated organ. As the number of MRIs performed increases, more pancreatic lesions are likely to be discovered. This makes our ability to differentiate between different lesion types – those with benign behaviour from the clearly malignant – of the utmost importance to diagnosis, treat and manage our patients.
In a patient with suspected pancreatic lesions the general imaging work-up starts with diffuse abdominal ultrasound, then a CT-scan to assess the whole pancreas. It is important to ascertain that the pancreas is normal in its morphology and in its relation to the rest of the gastro-intestinal organs. CT is also useful for finding evidence of calcification. Further assessment of the pancreatic ducts, biliary system and surrounding parenchyma is then performed using MRI where higher contrast resolution facilitates imaging of the important relationship between the cystic lesion and the pancreatic ducts.
What types of pancreatic lesions are there and how can they be differentiated?
The majority of pancreatic cystic lesions will be pseudocysts which express benign behaviour and often result from acute inflammation of the pancreas (pancreatitis) and/or surrounding tissues. Of greater concern are neoplastic cysts. The three most important pancreatic tumour types are intraductal papillary mucinous neoplasm (IPMN), mucinous cystic neoplasm (MCN) and serous cystic neoplasm (SCN). Again the whole pancreas, especially the ductal system and its relationship with the lesion has to be taken into account in identifying these lesions and imaging by either CT or MR is important to determine this.
By their nature, IPMN is a tumor that can occur within the cells of the pancreatic duct. IPMN tumors often produce mucus. Although IPMNs are benign tumors, they can progress to pancreatic cancer. Here, imaging is of great assistance in the asymptomatic patient for deciding whether resection should be performed or not. If the lesion is in a side branch of the main duct and there are no other signs of malignancy, then observation for life, with regular follow-up is a viable option for management.
If there is no ductal communication, the lesions are likely to be either MCN or SCN. The former group, generally solitary cysts, was once always treated by resection. However, advances in our understanding have enabled us to conclude that only a subset of these tumours are malignant or premalignant and for the main part, when patient demographics, symptoms and other clinical findings are considered, these lesions can be managed with frequent follow-up, rather than surgery.
SCN can be considered as purely benign and unless they become greatly enlarged and cause pain by compression do not require resection.
Do they affect both genders equally?
There is a clear gender distinction for the type of pancreatic cystic lesion found. IPMN is most frequently diagnosed in men, particularly middle-aged men, whereas mucinous and serous cysts are more common in women. Only MCN have clearly been defined by the presence of ovarian stroma at a rate of approximately 9:1. In the other lesion types, the reason for the clear gender differences that exist is not yet understood.
What particular challenges are encountered in the diagnosis of these lesions?
For a good diagnostic work-up we need to consider the whole picture in front of us and not rely on just one technique or result
Valérie Vilgrain
Accurate diagnosis is essential for correct patient management. Therefore, it is particularly challenging to get it right. For a good diagnostic work-up we need to consider the whole picture in front of us and not rely on just one technique or result. Patient, age, family history, sex, clinical background and co-morbidities etc. are all of importance in the diagnostic procedure and when considering management options. Histology is not a reliable option in cystic lesion differentiation but the imaging modalities of CT and MR are essential, and complementary, in identifying the nature of the lesion, position, size, calcification, nodule, wall thickness and of course its relation with the pancreatic ducts. Endoscopic ultrasound, performed under general anaesthetic, is a more invasive technique and generally not performed early in the patient journey. Biochemical analysis of the cystic fluid is of highest utility to differentiate between mucinous and non-mucinous lesions but is unable to distinguish between invasive and non-invasive MCN. We are now fortunate to have some accurate biomarkers such as CEA, CA 19-9, CA 72-4 that form a panel of highly specific markers.
What is the main message you hope to convey at the upcoming CT conference?
My main message is the importance of correctly integrating imaging into the diagnosis of these lesions. That CT and MRI are truly complementary techniques that both have an important place within a wider clinical picture as clearly defined in recent European Clinical Guidelines for the successful identification and management of pancreatic cystic lesions.
Profile:
Professor Valérie Vilgrain is an expert in abdominal imaging specialising in liver, biliary and pancreatic diseases at Hôpital Beaujon, Hôpitaux Paris-Nord Val de Seine in Clichy, France. Her main research interests are diagnostic and interventional imaging of the liver, pancreas and bile ducts with a particular interest in multidetector CT and MRI. She is Director of ESOR (European School of radiology) and member of several national and international societies, such as the RSNA (Radiological Society of North America), ESR (European Society of Radiology), ESGAR (European Society of Gastrointestinal and Abdominal Radiology), EASL (European Association for the Study of Liver) and SFR (French Radiological Society). Professor Vilgrain has published 430 peer-reviewed papers and has been principal investigator of several large multicentre clinical trials. She is currently on the Editorial Board of Journal of Hepatology and Abdominal Radiology and is a reviewer for a number of renowned journals.
Presentation:
Freitag, 24.01.2020, 10.50-11.10 Uhr
Cystic lesions of the pancreas
Valérie Vilgrain (Clichy, Frankreich)
Session: Onkologie
24.01.2020