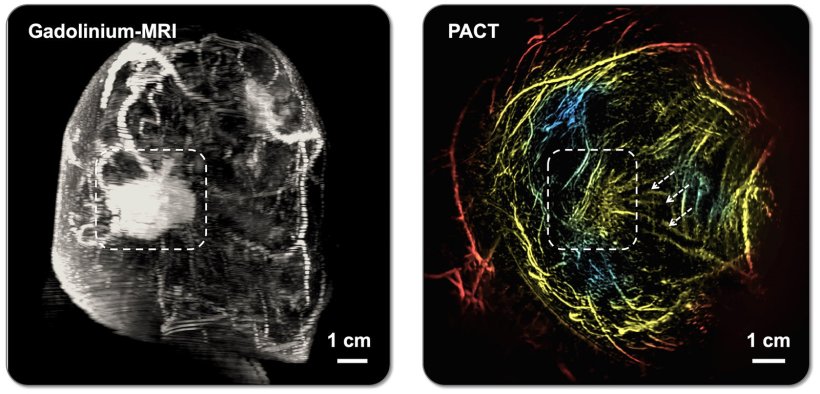
Image credit: Xin Tong/Caltech Optical Imaging Laboratory
News • Photoacoustic computed tomography
PACT: AI-assisted edge in breast imaging
A team led by the California Institute of Technology (Caltech) has developed a safe, effective, and painless breast imaging technique that incorporates machine learning to help differentiate between suspicious and healthy tissue.
The method has now been tested on patients and performs as well as or better than other conventional breast imaging techniques.
For decades, X-ray mammography has been the gold standard of breast imaging for the early detection of breast cancer. While the technique remains valuable in terms of reducing cancer deaths, it does expose patients to small amounts of ionizing radiation, painfully squeezes breasts to allow X-rays to more easily pass through tissue, and, especially in the case of dense breast tissue, produces many false positive diagnoses.
We'd like to make PACT a clinical tool that benefits patients—to help detect breast cancer without patients taking the risk of getting cancer or worrying about an allergic reaction
Lihong Wang
Other techniques such as ultrasound and magnetic resonance imaging (MRI) can be used for breast imaging, but these also have problems. Ultrasound is very safe, but its accuracy is dependent on the skill of the operator and the results are not always conclusive. MRI is time-intensive, expensive, and cannot be used on patients who are allergic to contrast agents or those who are claustrophobic or have certain implants. "We were strongly motivated to work on this problem because none of the current techniques are perfect," says Lihong Wang, the Bren Professor of Medical Engineering and Electrical Engineering at Caltech. "The future of medicine has to be better than that."
The technique that Wang and his colleagues have developed and refined over the past 20 years is called photoacoustic computed tomography, or PACT. It offers a breast imaging alternative without the discomfort, high costs, or risk associated with the conventional evaluation methods. PACT features a laser-sonic scanner that can identify tumors in as little as 15 seconds.
Working with researchers at the City of Hope Comprehensive Cancer Center in Duarte, California, the team has tested PACT on 39 patients. It achieved comparable results to mammography and MRI in terms of differentiating between suspicious and normal tissue as well as malignant and benign growths or lumps.
The scientists describe PACT and their clinical results in a new paper in the journal Nature Biomedical Engineering. The lead authors of the paper are Xin Tong (MS '21), Cindy Z. Liu, and Yilin Luo, graduate students in the Andrew and Peggy Cherng Department of Medical Engineering at Caltech; along with Li Lin (PhD '20), who completed the work while at Caltech and is now at Zhejiang University in China.
Recommended article
News • Breast cancer
New imaging technique to ensure surgeons completely remove cancer
Of the quarter-million women diagnosed with breast cancer every year in the United States, about 180,000 undergo surgery to remove the cancerous tissue while preserving as much healthy breast tissue as possible. However, there’s no accurate method to tell during surgery whether all of the cancerous tissue has been successfully removed.
"This is the culmination of literally decades of work," says Wang, who is also the Andrew and Peggy Cherng Medical Engineering Leadership Chair and executive officer for medical engineering at Caltech. "We'd like to make PACT a clinical tool that benefits patients—to help detect breast cancer without patients taking the risk of getting cancer or worrying about an allergic reaction."
PACT works by shining a near-infrared laser pulse into the breast tissue. The laser light diffuses through the breast and is absorbed by molecules. For example, it can be absorbed by oxygen-carrying hemoglobin molecules in the patient's red blood cells, causing the molecules to vibrate ultrasonically.
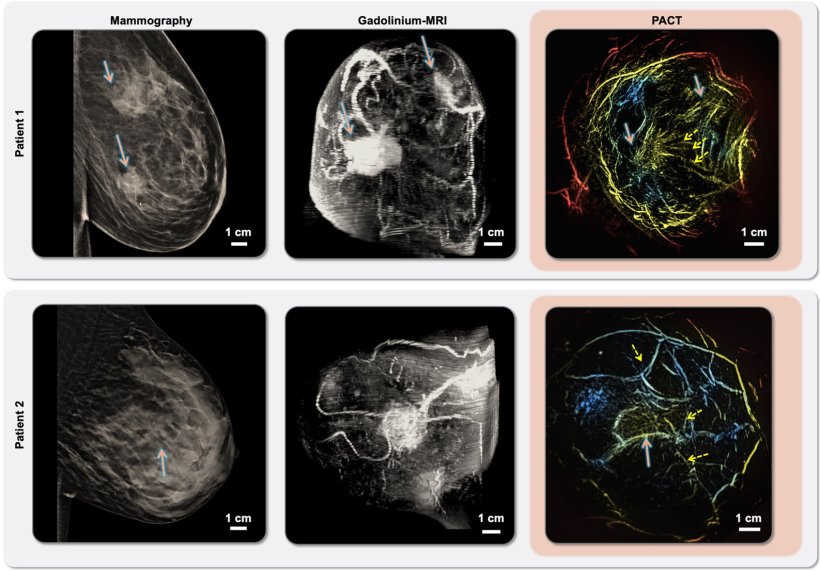
Image credit: Xin Tong/Caltech Optical Imaging Laboratory
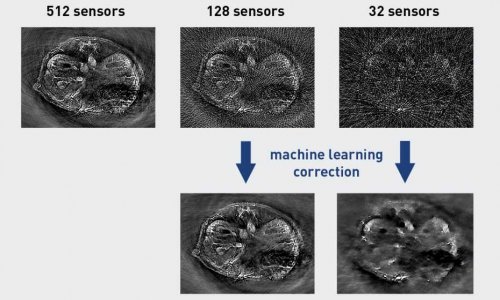
Unlike X-rays, which travel in a straight line, light waves scatter, or bounce around inside tissues, making it difficult to get high-resolution images. So PACT combines light and sound into a single modality. "We use light to see the molecules, but we use sound to define the spatial location," Wang says.
The vibrations from the molecules travel through the tissue and are picked up by an array of 512 tiny ultrasonic sensors placed over the skin of the breast. Data from those sensors are used to assemble an image of the breast's internal structures in a process that is similar to ultrasound imaging, though much more precise. PACT can provide a clear view of structures as small as a quarter of a millimeter at a depth of 4 centimeters.
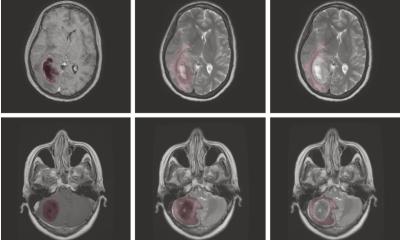
"We basically use molecules to figure out the body's physiology," Wang says. "That's the beauty of photoacoustic tomography: By detecting molecules, we can figure out exactly how the body is functioning. When there's a functional difference, that means we can potentially detect disease better." For example, PACT is excellent at detecting hemoglobin and therefore revealing angiogenesis, a common signature of breast cancer that involves the growth of additional blood vessels to deliver more nutrient-rich blood to cancerous cells. PACT can also detect tumor hypoxia, another signature of cancer, where fast metabolism outstrips the blood supply, leaving parts of the tumor starved of oxygen.
With the maturity of artificial intelligence (AI) and machine learning, Wang says PACT has become better at detecting abnormalities in breast tissue than it was a few years ago. The scientists trained the system on images of malignant and benign growths or lumps as well as suspicious and healthy tissue, improving its ability to notice subtle variations that indicate what type of tissue has been imaged. Indeed, Wang says, PACT can often detect problematic features that would likely go unnoticed by the human eye.
During a PACT scan, the patient lies face down on a table with a recess containing a warm water bath, ultrasonic sensors, and the laser. One breast at a time is placed in the recess, and the laser shines into it from below. Because the technique is rapid, each scan can be accomplished while the patient holds their breath. "We started with a basic lab system—just a single-element ultrasound transducer that we rotated around—and it took forever. Now we can do 3D imaging during a single breath, making it very practical," Wang says.
Wang adds that in some ways, the new work is just the beginning, as the team believes it will be able to further enhance the technique's imaging quality by adding additional laser wavelengths to the two they currently use and improving additional features. Looking to the future, the team's next steps include acquiring a larger dataset from additional breast cancer volunteers, improving the classification model by leveraging more features, and eventually commercializing the technology.
Source: California Institute of Technology; written by Kimm Fesenmaier
03.07.2025