Image credit: Antonio Tabernero / CNIO
Interview • Congress showcases advances
Making immunotherapy work for more cancer patients
Three experts explain how research is being done to make immunotherapy effective in an increasing number of breast cancers
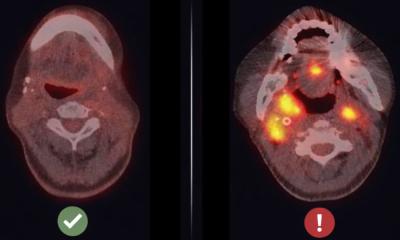
Immunotherapy has become the most promising strategy for treating cancer, but its effectiveness is still very uneven. In the month of breast cancer, the most common tumor in women – almost 2.5 million cases are diagnosed worldwide each year –, three researchers present the main advances and challenges in the application of immunotherapy to this tumor at the Spanish National Cancer Research Center (CNIO).
Karin de Visser (Netherlands Cancer Institute, Amsterdam), Dr. Sandra Demaria (Weill Cornell Medicine, USA) and María Casanova-Acebes (CNIO) are participating in the cancer immunotherapy congress being held this week at the CNIO, with the support of the ‘la Caixa’ Foundation. De Visser is investigating the relationship between the immune system and metastatic breast cancer, and is designing new immunomodulatory strategies to combat this type of tumor. Demaria has shown that radiotherapy, in addition to killing tumor cells, can recruit the immune system to fight cancer. Casanova-Acebes is head of the Cancer Immunity Group at the CNIO; she studies the influence of biorhythms on the immune system and their relationship with cancer.
Is immunotherapy effective in breast cancer today?
De Visser: “It depends on the type of breast cancer and how advanced it is. For example, in triple-negative breast cancer, immunotherapy works in between 20% and 30% of patients.”
Do we know why it works in some patients and not in others?
Triple negative is more frequent in obese people, and yet in this type of cancer immunotherapy works better in patients with a higher body weight, and this is something we do not see in other tumors
María Casanova-Acebes
De Visser: “We don’t know, and finding out is the key to progress. So far, we treat patients homogeneously, and we need to move to more personalized immunotherapy. There is a lot of ongoing research to understand what is special about patients who respond, and how to learn from this knowledge to apply it to non-responders.”
Casanova-Acebes: “We know that there are contributing factors. For example, triple negative is more frequent in obese people, and yet in this type of cancer immunotherapy works better in patients with a higher body weight, and this is something we do not see in other tumors. This tells us that understanding how factors such as diet and other risk factors such as the disruption of sleep-wake rhythms play a role is important. Part of the explanation for the different responses may lie in these factors.”
Is this emphasis on factors such as diet and biorhythms new?
Casanova-Acebes: “We are only now beginning to pay attention to the fact that immunotherapy has a systemic effect, it affects the whole organism, and that other factors that confer risk (such as certain diets or alterations in biorhythms) can limit its efficacy.”
What do we know about the best diet to prevent breast cancer?
Demaria: “We are seeing that diet and microbiome are important. We can say, for now, that the best diet is a fiber-rich one. This is because the intestinal flora, the microbiome in our gut, is in constant communication with the rest of the body, and the immune system works better if we have the right bacteria. And these bacteria like fiber.”
How does more knowledge help immunotherapy reach more patients?
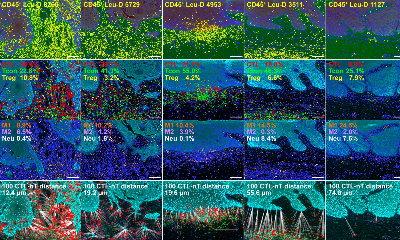
De Visser: “For example, until now immunotherapy has worked by activating only one type of cell, the T-lymphocytes. But the immune system is much richer, and in fact in breast cancer there are not so many T lymphocytes involved, but other cells of the immune system, such as myeloid cells. We have to understand the relationship between all these cells, and how to act on them in order to have a response against the tumor.”
Demaria: “Much remains to be done, but we are learning a lot about how to use immunotherapy. For example, the checkpoint inhibitors approved so far suppress some of the immune system’s brakes [and by suppressing them they strengthen the body’s attack on the tumor], but there are many more points to act on, such as myeloid cells that are very diverse and abundant in metastasis.”
What will happen in the next ten years in this area?
We will move toward more precise therapies, guided by specific biomarkers. [...] Tthe key is to understand what makes each patient’s response the way it is
Sandra Demaria
De Visser: “I think that, as is already the case with melanoma, in breast cancer immunotherapy will be given before, not only after, other alternatives. We will also see better responses and have other types of immunotherapy for breast cancer, not just checkpoint inhibitor-based immunotherapy as now. And they will be more personalized: we will be able to predict the most effective strategy for each patient. That is where we are making progress in research.”
Demaria: “We will move toward more precise therapies, guided by specific biomarkers. Now there are patients who really benefit from a therapy that is being tested, but the trial is considered failed because there are few favorable responses. So the key is to understand what makes each patient’s response the way it is.”
Casanova-Acebes: “It will also be important to know how to reduce side effects, which also exist in immunotherapy.”
It would seem that, having obtained the first successes in immunotherapy, more knowledge must now be gathered before the advances can reach more patients.
De Visser: “The results that immunotherapy has brought to the clinic are very promising. In melanoma and in some types of breast cancer, immunotherapy works well in certain patients, but now many alternatives remain to be investigated to make it work for many more patients. We must not forget that current successes come after centuries of basic research to understand how the immune system works. What is being achieved now is spectacular, we are curing patients who a decade ago had no alternative, and now our task is to make it work for more patients.”
Source: Spanish National Cancer Research Center
22.10.2024