Adapted from: Su Y, Ouchi R, Daroonpan P et al., Cancer Immunology, Immunotherapy 2025 (CC BY 4.0)
News • Stratification of TSCC immunotypes
Tongue cancer: Immune profiling for improved outcomes
Classification of immune profiling on tumor samples helps explain improving treatment outcomes, paving the way for personalized tongue cancer medicine
Immunotherapies are transforming the landscape of cancer treatment worldwide. By harnessing the body’s immune system to fight disease, they can achieve outcomes in advanced cancers that are impossible with conventional methods. However, these therapies don’t work equally well for all patients and cancer types.
For example, despite the promise of immune checkpoint inhibitors (ICIs)—drugs that cancel inhibitory signals to effector T cells—their effectiveness against head and neck squamous cell carcinoma (HNSCC) has been disappointing. While these therapies yield impressive results in melanoma and lung cancer, only about 10% of patients with HNSCC experience durable responses. Tongue squamous cell carcinoma (TSCC), the most common type of oral cancer, is particularly challenging due to the tongue’s continuous exposure to environmental stimuli and immunotolerant status.
Shedding light on this issue, a research team led by Professor Miyuki Azuma from Institute of Science Tokyo, Japan, expanded a TSCC cohort of comprehensive immune profiling analyses, published in the previous paper in Oral Oncology, and conducted classification of TSCC immune profiling, published online in Cancer Immunology, Immunotherapy.
We expect the results of this study to promote personalized medicine in tongue cancer, enabling the selection of optimal treatments for more patients and contributing to improved treatment outcomes
Miyuki Azuma
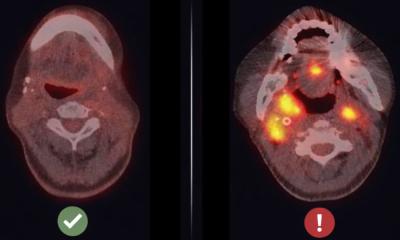
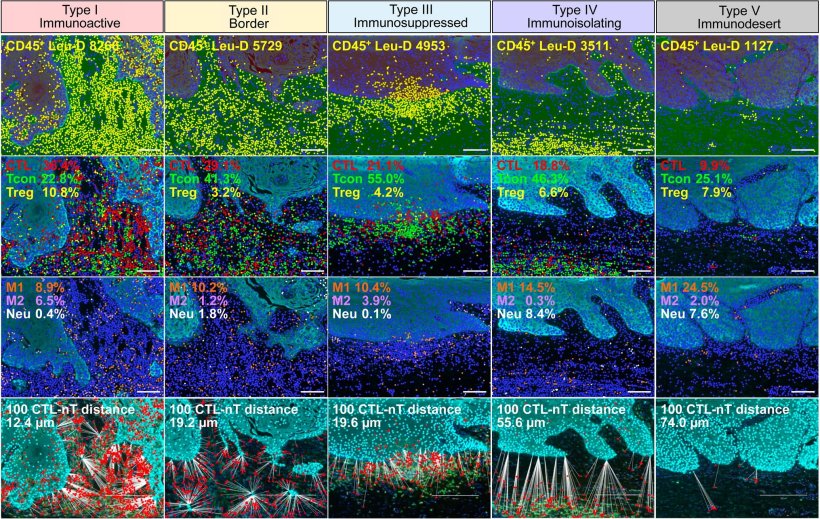
The researchers employed advanced multiplex immunofluorescence and tissue imaging techniques to analyze the presence and distribution of various immune cells within tumors. They also conducted spatial analysis to quantify distances between tumor cells and cytotoxic T lymphocytes, an important subtype of immune cells that can kill cancer cells.
Based on the gathered data and statistical analyses, the team identified five distinct immunotypes. Immunoactive type I profiles would likely respond well to current immunotherapies. In contrast, immunosuppressed type III showed active suppression of immune responses, and immunoisolating type IV featured immune cells that were unable to engage with cancer cells. Finally, immunodesert type V was marked by an almost complete lack of immune cell infiltration. “We found that the immunoactive type, which would be sensitive to ICI monotherapy, was rare, and most TSCC cases exhibited immune-regulated immunotypes,” explains Prof. Azuma. Specifically, about 70% of untreated TSCC tumors fell into types III–V, explaining why current immunotherapies targeting programmed cell death protein often fail.
Additionally, the researchers found that tumor-node-metastasis staging, a traditional cancer classification system, cannot accurately predict a tumor’s immune profile. This finding highlights the need for immune-based assessments to guide treatment decisions. The team believes that the immunotype classification system could help clinicians identify patients who can benefit from immunotherapy alone versus those who need combination approaches. For example, patients with type I tumors might respond well to standard ICIs, while those with types III–V might require additional interventions to overcome immunosuppression. “We expect the results of this study to promote personalized medicine in tongue cancer, enabling the selection of optimal treatments for more patients and contributing to improved treatment outcomes,” concludes Prof. Azuma.
Overall, this study represents an important step toward precision oncology for patients with TSCC, potentially improving treatment responses and guiding them toward successful immune landscape-based therapies.
Source: Institute of Science Tokyo
31.05.2025