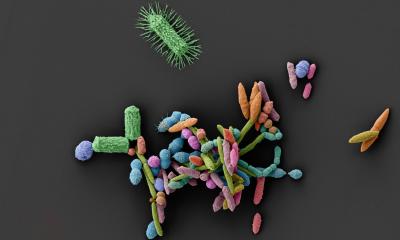
Image source: GIMM
News • When good bacteria fight back
Klebsiella strain to protect against IBD gut infections
A team of researchers led by Karina Xavier has uncovered a promising new live biotherapeutic agent that may redefine how the medical field approaches microbiota-based therapies.
Their study, published in Nature Communications, demonstrates that a harmless strain of Klebsiella – originally discovered by chance in laboratory experiments – can eliminate infections and reduce gut inflammation in mouse models of inflammatory bowel disease (IBD).
The bacterium, Klebsiella sp. ARO112, named after PhD student Ana Rita Oliveira, belongs to the same family as the hospital-associated pathogen Klebsiella pneumoniae but is inherently non-pathogenic. Instead of causing disease, this naturally occurring gut microbe helps restore microbial balance and prevents colonization by dangerous bacteria such as pathogenic Escherichia coli and Salmonella.
Not only did the bacterium eliminate the infection, but it also helped the microbiota regain balance much faster
Karina Xavier
The breakthrough began when the team noticed something unusual in their antibiotic-treated mice: animals carrying ARO112 showed remarkable resistance to infection. Initial findings, published in Nature Microbiology in 2020, revealed that this harmless Klebsiella competes for nutrients and ecological niches in the gut, blocking harmful bacteria from multiplying. The new Nature Communications study takes this a step further, with Vitor Cabral and Rita Oliveira from the Xavier lab, exploring the bacterium’s therapeutic potential in a mouse model carrying a genetic mutation associated with human IBD.
When microbiota-impaired mice were treated with ARO112 after antibiotic exposure and infection with pathogenic E. coli, the results were very surprising: near-total clearance of infection, far greater than seen in previous models; accelerated recovery of the microbiota, enabling beneficial bacteria to resume production of protective metabolites such as butyrate; and significant reduction of intestinal inflammation. “This time we observed total clearance”, says Xavier. “Not only did the bacterium eliminate the infection, but it also helped the microbiota regain balance much faster”.
The team also compared the strain with E. coli Nissle 1917, a well-known commercial probiotic widely used in Europe. Nissle showed no protective effect under these conditions – highlighting that some probiotics work only in specific microbial ecosystems, and new tailored solutions are needed.
Given the notoriety of some Klebsiella species, the researchers conducted extensive safety assessments in collaboration with the laboratory of Carles Ubeda, from the Foundation for the Promotion of Health and Biomedical Research of the Valencian Community (Fisabio). The results were unexpectedly reassuring: ARO112 does not produce biofilms; It does not easily acquire antibiotic resistance genes, and even when artificially given a resistance plasmid, it naturally loses it within days. Its presence in the gut is temporary – as the microbiota recovers, ARO112 naturally disappears. “In evolutionary terms, it behaves like a volunteer firefighter”, Xavier explains. “It fills a gap, restores balance, and then steps aside”.
ARO112 represents a new class of next-generation probiotics – not derived from food sources, like traditional lactic acid bacteria, but directly isolated from the microbiota of healthy mammals. Such targeted live biotherapeutics could one day be used after antibiotic treatments to prevent infections and reduce inflammation, offering a precise alternative to broad procedures like fecal transplants. Recognizing this strong potential for clinical translation, GIMM’s Funding & Innovation Team is advancing the valorization pathway for ARO112, including technology maturation, regulatory landscaping, and strategic outreach to industry. “We’ll always need antibiotics,” says Xavier. “But they disrupt the microbiota. Imagine a future where you take an antibiotic and then follow it with a bacterium like ARO112 to restore balance. That’s the promise of next-generation microbiome therapies.”
Source: GIMM – Gulbenkian Institute for Molecular Medicine
18.12.2025