Article • Predictive biomarkers
Immunotherapy follow-up with MRI: the search is on
Immunotherapy is taking center stage in imaging, but patient follow-up with CT is no cookie and may fall short in the peripheral limbs, brain and bone marrow. MRI offers specific benefits in these situations, and, combined with PET, it may bring even more results.
Report: Mélisande Rouger
Research must be carried out on quantitative techniques and tracers developed to fully exploit that potential, Prof. Dow-Mu Koh (Sutton/UK) explained in the deciated New Horizon session Friday at ECR. The role of imaging is to assess treatment response, predict response and patient benefit, identify complications, offer disease prognosis and evaluate disease relapse, Koh said. However, in practice, things are a little different. “We are quite far of achieving these objectives,” the researcher said.
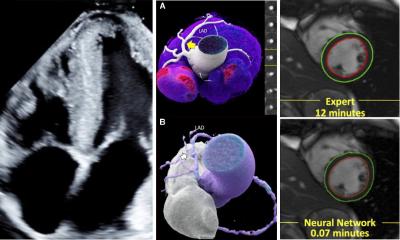
MRI techniques provide morphological and functional imaging, and even the potential for hybrid imaging. Researchers are focusing on how to use soft tissue contrast of MRI to enhance disease assessment, especially in those sites of disease that are poorly visualized with CT. “MRI is useful in areas not naturally included by CT studies, for instance peripheral limb. Small brain metastases can be challenging for CT, and so can be disease confined to the bone marrow,” Koh said.
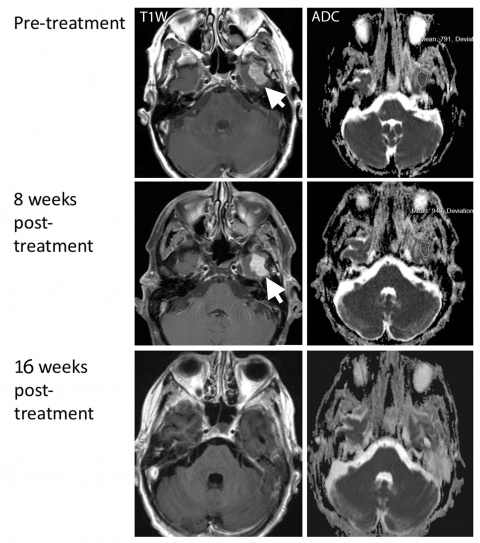
Current criteria iRECIST allows responses not typically observed in traditional systemic treatment to be identified and better documented.The new guidleine, which was introduced a year ago, notably gives the opportunity to classify assessments after i-unconfirmed progressive disease (iUPD) has occurred – with following disease progression confirmation in 4-8 weeks time. Radiologists must especially be ware of the challenges inherent to follow-up imaging within this time. “What we’re observing at 8 weeks is pseudo progression or the so-called flare reaction,” Koh said. The situation that needs to be imaged with MRI is usually more complex than on CT, he added. “Lesions can grow… In our research we noted a decrease after 16 weeks, and after 24 weeks the lesion was totally gone.”
Radiologists must also be able to recognize and visualize immune related events, and one of MRI’s strengths is to look for the presence of hypophysitis, Koh noted. “We know that this has higher incidence with CTLA-4 blockade; it has a reported incidence of 17%, and may be associated with pituitary failure associated with low ACTH and TSH levels. Often the patient would present with fatigue and headaches,” he said.
Brain MRI is currently the best test to look at changes in pituitary gland. “What you are looking for is symmetrical diffuse enlargement of pituitary gland and thickened undisplaced pituitary stalk without any sellar erosions. It’s really important to assess these changes as early as possible because established hypophysitis is irreversible and the patient would have to be placed under life-long hormone therapy,” Koh said. Another benefit of MRI is that it does not utilize ionizing radiation, so it can be often repeated in the follow-up of patients. But MRI does have limitations, and the most important is the absence of any confirmed prediction prognostic MRI biomarkers for immunotherapy. “The search is on as to what we can use to predict which patients would benefit from that kind of treatment,” Koh said.
Despite an increasing number of studies, it remains hard to predict whether one might be dealing with either pseudo-progression, hyper-progression or concealed response on MRI. It is generally accepted that the overall rate of pseudo-progression is less than 10%, and that this process could be due either to infiltration of the tumor site by immune cells or continued tumor growth until a sufficient response develops. In hyper-progression, radiologists can usually observe accelerated tumor growth during treatment. HP is also associated with poorer survival, according to Koh.
The idea is to develop PET imaging tracers that can identify and predict treatment response, which can be explored alongside multi-parametric MRI measurements on a MRI/PET hybrid system as imaging biomarkers
Dow-Mu Koh
Another key limitation for morphological MRI is that it really doesn’t allow spotting changes in the lungs. “Changes such as pneumonitis will always be better appreciated on CT,” he said. There is a lot of interest to see if radiologists can use other views of MRI techniques to get better functional information. “MRI techniques result in quantitative measurements, which reflect different aspects of disease pathophysiology. We have DWI, CE MRI… and we also have magnetization transfer MRI, which is very interesting to assess immunotherapy,” he said. Magnetization transfer MRI is the process by which macromolecules and their associated water molecules cross-relax with protons in the free water pool. Their interaction can be measured by applying radio frequency to the pool, using the off-resonance MR pulse.
Research on all these techniques is ongoing to increase contrast between tissues. Hybrid imaging could also be of tremendous help, but PDG PET may show false positive result at follow-up because of the flare response. Novel tracers are therefore being explored, namely N-(2-(diethylamino)-ethyl)-4-18F-fluorobenzamide (18F-FBZA), 64CU-Radiolabeled HAC-PD1, 64CU-Radiolabeled DOTA-CTLA4, and 68Ga-NOTA-GZP. “The idea is to develop PET imaging tracers that can identify and predict treatment response, which can be explored alongside multi-parametric MRI measurements on a MRI/PET hybrid system as imaging biomarkers,” Koh said.
How long this will take yet remains to be determined.
Profile:
Dow-Mu Koh MD is consultant radiologist in functional imaging and Professor for functional cancer imaging at the UK’s Royal Marsden Hospital and its academic partner The Institute of Cancer Research (ICR). His research focuses on functional imaging techniques for tumour assessment.
04.03.2018