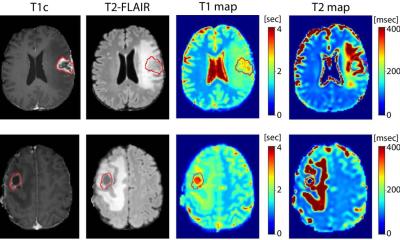
Image credit: Cambridge University Hospitals NHS Foundation Trust
News • Pandemic-induced treatment delays
“Heartbreaking”: the impact of Covid on children with brain tumours
The first ever investigation into the impact of the Covid pandemic on children and young people with brain tumours has revealed how investigations or treatments were frequently postponed as key people or resources were not available.
The study in the British Medical Journal Open was led by Lancaster University and Cambridge University Hospitals NHS Foundation Trust with Manchester University, Manchester University NHS Foundation Trust and Nottingham University Hospitals NHS Foundation Trust.
Paediatric brain tumours are the second most common childhood cancers, with around 500 children and young people diagnosed each year in the UK. Delays in diagnosis can make treatment more complex and increase the likelihood of death or disability. However, diagnosis is often difficult, as symptoms and signs can be non-specific - often picked up in optometry, primary care, nurseries and schools, all of which were also disrupted during the pandemic.
Overall, this study not only sheds light on the challenges faced by families during the pandemic but also provides suggestions for improving healthcare services to ensure a more comprehensive and effective response in times of crisis
Rachel Isba
The study, funded by Action Medical Research for Children, involved interviewing parents and caregivers, children and young people, clinical staff and charities throughout the UK between January 2022 and June 2023.
Dr Liz Brewster of Lancaster University said: “In this research, families shared such heartbreaking stories of their children undergoing treatment during the pandemic.” The principal investigators were Mr Ibrahim Jalloh, an Addenbrooke’s consultant neurosurgeon and Professor Rachel Isba, from Lancaster Medical School and Alder Hey Children’s Hospital where she is a consultant in Paediatric Public Health Medicine. Professor Isba said: “Overall, this study not only sheds light on the challenges faced by families during the pandemic but also provides suggestions for improving healthcare services to ensure a more comprehensive and effective response in times of crisis.”
Lockdown meant that seeing a GP face-to-face was more difficult and remote consultations relied on clear caregiver reporting to ensure that ‘red flags’ were noted. One caregiver said: “A lot of them were telephone consultations. They wouldn't actually see us because of Covid. … If you explain stuff over the phone, they're just agreeing with you. They're just taking your point of view.” Children were not seen in other settings such as nursery, school or social situations, making it harder for caregivers to evaluate their concerns. One specialist nurse said: “I think we had a couple of delayed presentations just because they had no idea that their child was different to anyone else. And it wasn't until they became quite sick, because that was then picked up when they brought the child to A&E.”
Caregivers felt they had to ‘stay strong’ for their child but were often traumatised by their own experiences, with infection control restrictions posing significant challenges. One caregiver said: ”When [daughter] came out of theatre, I wasn't allowed to go and see her, because I wasn't the designated parent. And it is heartbreaking, absolutely heartbreaking, to not be able to go and see that your child is okay.” Dr Brewster said: “It’s vital we use the insights from their experiences to learn how to manage healthcare in challenging circumstances to improve for the future.”
Source: Lancaster University
07.01.2025