MEDICA 2013
Genetically targeted medicine forges ahead
Healthcare is undergoing a major change set to offer a real prospect of far more genetically targeted treatments, according a leading human geneticist Sir John Burn, Professor of Clinical Genetics at Newcastle University, England.


In his keynote speech entitled Personalised Care, to be presented at the Medica Education Conference 2013 (21 November), Sir John will re-buff any cynicism over personalised medicine ever having a role in healthcare. He will outline just how genome analysis detects an individual’s genetic predisposition for certain diseases and how better assessment of their prognosis will play a greater role as personalised medicine takes the lead.
Ahead of the Dusseldorf conference, during our European Hospital interview he said: ‘I need to get across to people that there has been a sea change technologically and that means there is now a real prospect of delivering a much more genetically-targeted form of healthcare.’
There is now better understanding of the molecular level of the diseases, particularly cancer, he explained, pointing out that scientists and clinicians can now find the explanation for rare genetic syndromes and identify people’s genetic predispositions to anyone of a myriad of disease virtually at will.
Doctors have to recognise that diseases once considered common are now rare and that rare conditions are ‘in relative terms more common’, Sir John said. ‘Rare diseases are now collectively a large chunk of our workload and now that we have the capacity to understand those diseases at a much more precise level and predict which ones will run in families, we are duty bound to get our heads round this in a way that collectively we have avoided before.’
This is being driven by the availability of targeted medication, he explained, and cited early examples such as treating chronic myeloid leukaemia by targeting the molecular basis of the tumour, and with B-raf mutation in melanoma, which opened the way for dramatic improvements in prognosis for patients with malignant melanoma. ‘These very expensive but highly effective drugs are targeted to individual patients, which will change the whole ground on which we operate. Up to now most genetic testing has been done in rare conditions and at the end of a long diagnostic chain,’ he pointed out. ‘What is happening, and is going to happen even more extensively, is that it will become the first thing you do, rather than the last thing, to investigate the genetic make-up.’
The shift, he continued, will also see geneticists move from looking at one gene at a time to capturing the fragments of all the genes they think are relevant to a specific disease and on to exome sequencing to capture fragments of all the genes in the coding sequences.
The ultimate step was to move to whole genome sequencing which has now fallen in price to a few thousand euros, Sir John said.
Problems that he plans to identify during his address include incidental findings that suggest an individual is at risk of a genetic disorder and knowing how to tell them about it; and the need to acknowledge that subtle variations in gene expression – an area he believes is grossly under-estimated even by experts in the field – may be very important. ‘Subtle variation in gene expression in many of the common diseases will not be about gross loss of gene function but will be about a particular set of genes being slightly dis-regulated and causing a discord, which is very difficult to demonstrate unless you have the most subtle understanding of gene expression,’ Sir John emphasised.
The professor also stated that interventions need not be expensive. For many years he has pioneered the use of Aspirin as a means of preventing cancer. ‘We proved in people at the highest genetic risk that taking two aspirins a day for two years cuts their risk of cancer by 60%,’ he pointed out.
His keynote speech will conclude with a focus on the UK’s 100,000 Genome Project, which will sequence the personal DNA code of 100,000 patients over the next five years to help lead to better and earlier diagnoses and personalised care. He believes a major challenge is to encourage the European Union to embrace the initiative.
‘Personalised medicine is so important that it won’t be called personalised medicine,’ he said. ‘It will just be called medicine. It will be so integral to what we do.”
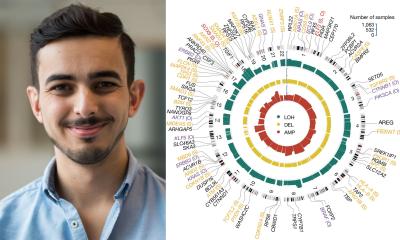
Profile:
Sir John Burn, Professor of Clinical Genetics at Newcastle University, England, was knighted in 2010 for services to medicine and healthcare. An Honorary Consultant Clinical Geneticist at Newcastle Hospitals NHS Foundation Trust, he was Lead Clinician NHS North East until March 2013 and chairs the Genetics Speciality Group (NIHR).
Meeting Today:
Professor Sir John Burn’s keynote lecture on Personalised Medicine will be delivered at the Medica Education Conference 2013, at 1pm on 21 November 2013, in CCD South, Room 3.
20.11.2013