© Kobe University (CC BY)
News • Functional connectivity imaging
fMRI brain scan predicts effectiveness of spinal cord surgery
A 10-minute brain scan can predict the effectiveness of a risky spinal surgery to alleviate intractable pain. The Kobe University result gives doctors a much-needed biomarker to discuss with patients considering spinal cord stimulation.
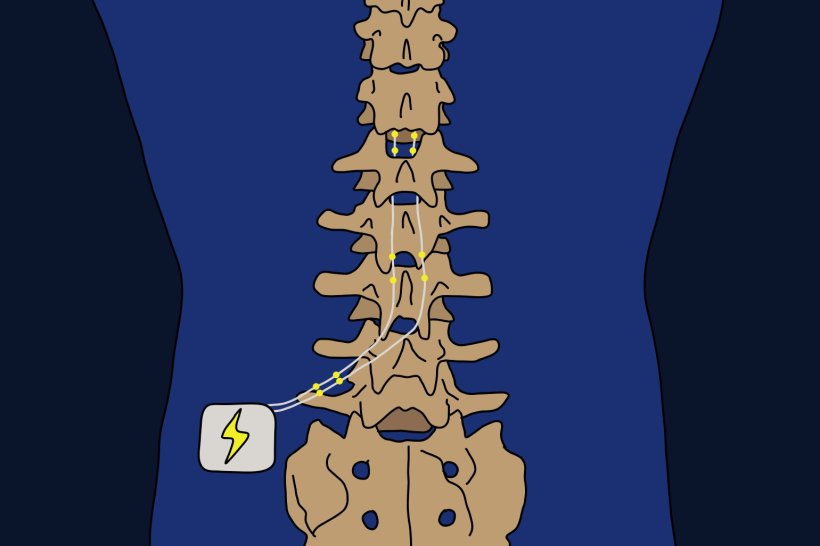
For patients with chronic pain that cannot be cured in any other way, a surgical procedure called “spinal cord stimulation” is seen as a method of last resort. The treatment works by implanting leads into the spine of patients and electrically stimulating the spinal cord. Because the spinal cord transmits sensations to the brain from all over the body, the position of the leads is adjusted so that the patients feel the stimulation at the site of the pain. The Kobe University anesthesiologist Kyohei Ueno says: “A big issue is that the procedure is effective for some but not for other patients, and which is the case is usually evaluated in a short trial of a few days to two weeks prior to permanent implantation. Although this trial is short, it is still an invasive and risky procedure. Therefore, clinicians have long been interested in the possibility of predicting a patient’s responsiveness to the procedure through non-invasive means.”
Ueno and his team published their results in the British Journal of Anaesthesia.
Not only does this offer an attractive biomarker for a prognosis for treatment effectiveness, it also strengthens the idea that an aberrant connection between these networks is responsible for the development of intractable chronic pain in the first place
Kyohei Ueno
Functional magnetic resonance imaging, or fMRI, has become a standard tool to visualize how the brain processes information. More precisely, it can show which parts of the brain are active in response to a stimulus, and which regions are thus functionally connected with each other. “In an earlier study, we reported that for the analgesic ketamine, pain relief correlates negatively with how strongly connected two regions of the default mode network are before the drug’s administration,” explains Ueno. The default mode network, which plays an important role in self-related thought, has previously been implicated in chronic pain. Another relevant factor is how the default mode network connects with the salience network, which is involved in regulating attention and the response to stimuli. Ueno says, “Therefore, we wanted to examine whether the correlation of the activities within and between these networks could be used to predict responsiveness to spinal cord stimulation.”
The team found that the better patients responded to spinal cord stimulation therapy, the weaker a specific region of the default mode network was connected to one in the salience network. Ueno comments, “Not only does this offer an attractive biomarker for a prognosis for treatment effectiveness, it also strengthens the idea that an aberrant connection between these networks is responsible for the development of intractable chronic pain in the first place.”
Undergoing an fMRI scan is not the only option. Combining pain questionnaires with various clinical indices has been reported as another similarly reliable predictor for a patient’s responsiveness to spinal cord stimulation. However, the researchers write that “Although the cost of an MRI scan is controversial, the burden on both patients and providers will be reduced if the responsiveness to spinal cord stimulation can be predicted by one 10-minute resting state fMRI scan.”
In total, 29 patients with diverse forms of intractable chronic pain participated in this Kobe University study. On the one hand, this diversity is likely the reason why the overall responsiveness to the treatment was lower compared to similar studies in the past and also made it more difficult to accurately assess the relationship between brain function and the responsiveness. On the other hand, the researchers also say that, “From a clinical perspective, the ability to predict outcomes for patients with various conditions may provide significant utility.” Ueno adds: “We believe that more accurate evaluation will become possible with more cases and more research in the future. We are also currently conducting research on which brain regions are strongly affected by various patterns of spinal cord stimulation. At this point, we are just at the beginning of this research, but our main goal is to use functional brain imaging as a biomarker for spinal cord stimulation therapy to identify the optimal treatment for each patient in the future.”
Source: Kobe University
06.12.2024