News • Improved patient response
Existing heart drugs may help with PD(L)1 immunotherapy
Researchers have found that a class of commonly-used heart drugs may also improve patients’ responses to anti-cancer immunotherapies called PD(L)1 inhibitors, according to preliminary findings to be presented at the 32th EORTC-NCI-AACR Symposium on Molecular Targets and Cancer Therapeutics.
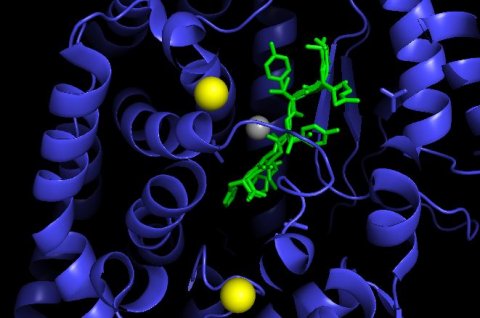
Angiotensin receptor II blockers (ARBs) are often prescribed for high blood pressure, heart failure, kidney failure and following a heart attack. They work by reducing the action of a chemical called angiotensin II, which plays a role in narrowing blood vessels and increasing blood pressure. ARBs block AT1 receptors that angiotensin II works on, and which are found in the heart, blood vessels and kidneys.
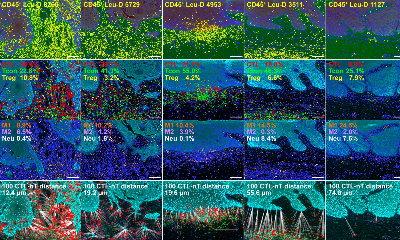
Dr Julius Strauss, co-director of the clinical trials group at the Laboratory of Tumor Immunology and Biology, at the USA’s National Cancer Institute’s Center for Cancer Research, presented this latest research. He said: “There are data suggesting that when angiotensin II, a protein in the body, binds to one of its receptors, AT1R, it has the potential to increase the levels of other proteins, VEGF and TGF beta, both of which have been linked to cancer growth and resistance to the immune system.”
The researchers thought that this overlap between the angiotensin II and the TGF beta pathways might mean that it plays a crucial role in the onset of cancer, its growth and also how cancer cells evade the immune system. “We decided to look at all the medications our patients were taking to see if any common medication or class of drugs might increase the likelihood of responding to anti-PD(L)1 treatment. After an initial review, ARBs seemed to be the most promising,” said Dr Strauss. He analysed data from 597 patients being treated with anti-PD(L)1 drugs in 20 clinical trials at the National Institutes of Health Clinical Center in the USA. The patients had more than three dozen different cancers, including prostate, lung, colon, ovarian, bladder and cervical cancers. Many were already taking ARBs or angiotensin-converting enzyme (ACE) inhibitors for heart problems unrelated to their cancer.
Recommended article

Article • The difficulty? Unpredictability in the entire process
Immunotherapy for lung cancer patients
Better outcomes, more favourable prognoses – oncologists and their lung cancer patients didn’t dare to dream about it. Finally, there might be hope. The so-called checkpoint inhibitors (immunotherapy drug) have been used successfully, albeit not for every patient. They are a double-edged sword, with risks as well as opportunities, as explained by Professor Cornelia Schäfer-Prokop.
Dr Strauss compared 71 patients who were taking ARBs together with their PD(L)1 inhibitor with those who were not. He also compared 82 patients receiving ACE inhibitors with those who were not. “Patients who were taking ARBs seemed to respond better and more often to anti PD(L)1 therapy for their cancer than patients who were not. We found that ARBs were associated with a statistically significant increase in the objective response rate as well as the complete response rate, compared to patients not taking ARBs,” he said.
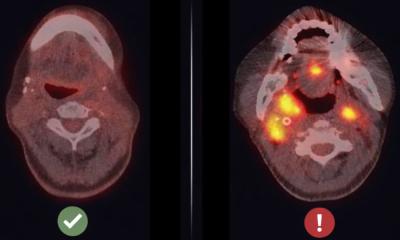
Among patients taking ARBs, the objective response rate (ORR), meaning the cancer had shrunk at least 30%, was 34% compared to 17% in patients not taking ARBs, while the complete response (CR) rate, meaning the cancer had shrunk 100% and could no longer be seen on scans, was 11% in patients taking ARBS compared to 3% in those who were not. However, there was no statistically significant improvement in ORR or CR rates among patients taking ACE inhibitors compared to those who were not taking them. Dr Strauss said: “The possible reason for the different effects seen with ARBs and ACE inhibitors might be that although angiotensin II increases levels of VEGF and TGF beta when it binds to the AT1R receptor, it can actually decrease levels of VEGF and TGF beta when it binds to another receptor, AT2R. Therefore, ARBs which selectively block just AT1R potentially work better at lowering VEGF and TGF beta levels than ACE inhibitors which block both AT1R and AT2R.
He continued: “In addition to ARBs potentially increasing the likelihood of responding to anti-PD(L)1 therapy, we also saw evidence that ARBs may help patients live longer. This beneficial effect of ARBS was seen in some cancer types more than others and was most notable in bladder cancer. However, these findings are very preliminary and other trials are needed to evaluate if ARBs may be beneficial to patients with cancer and to determine what, if any, cancer types may benefit the most, particularly in combination with anti-PD(L)1 therapy.”
Professor Udai Banerji, a member of the scientific committee for the Symposium and Deputy Director of the Drug Development Unit at The Institute of Cancer Research and the Royal Marsden Hospital in London (UK), was not involved with this research. He commented: “This hypothesis-generating population-based study offers interesting insights into the role of the interaction of the immune and cardiovascular system in promoting cancer. There is room for improvement for the clinical efficacy of immune checkpoint inhibitors, such as anti-PD(L)1 therapies. If these findings are validated in preclinical experiments and clinical trials this would be a tremendous opportunity to repurpose existing cardiovascular drugs to be used in combination with immune checkpoint drugs to improve outcomes of cancer patients.”
Source: European Organisation for Research and Treatment of Cancer (EORTC)
22.10.2020