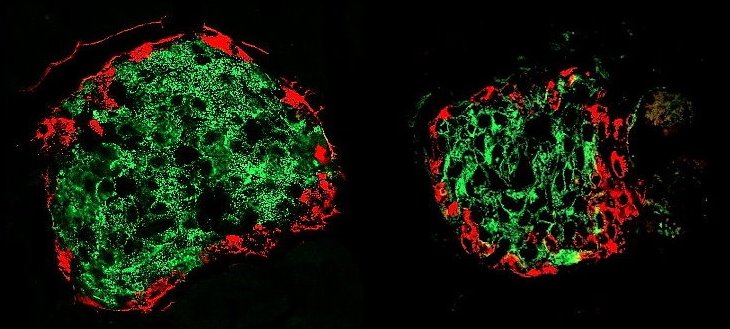
© UNIGE - Laboratory of Prof. Pierre Maechler
News • Early clues in the panceas
Detecting diabetes before first symptoms appear
A team from the University of Geneva in collaboration with Geneva University Hospitals (HUG) has discovered a molecule that can identify the development of diabetes before the first symptoms appear.
Diabetes is a severe and growing metabolic disorder. It already affects hundreds of thousands of people in Switzerland. A sedentary lifestyle and an excessively rich diet damage the beta cells of the pancreas, promoting the onset of this disease. If detected early enough, its progression could be reversed, but diagnostic tools that allow for early detection are lacking. A team from the University of Geneva in collaboration with several other scientists, including teams from the HUG, has discovered that a low level of the sugar 1,5-anhydroglucitol in the blood is a sign of a loss in functional beta cells. This molecule, easily identified by a blood test, could be used to identify the development of diabetes in people at risk, before the situation becomes irreversible. These results can be found in the Journal of Clinical Endocrinology & Metabolism.

© UNIGE
In Switzerland, almost 500,000 people suffer from diabetes. This serious metabolic disorder is constantly increasing due to the combined effect of a lack of physical activity and an unbalanced diet. If detected early enough at the pre-diabetes stage, progression to an established diabetes can be counteracted by adopting an appropriate lifestyle. Unfortunately, one third of patients already have cardiovascular, renal or neuronal complications at the time of diagnosis, which impacts their life expectancy.
‘Identifying the transition from pre-diabetes to diabetes is complex, because the status of the affected cells, which are scattered in very small quantities in the core of an organ located under the liver, the pancreas, is impossible to assess quantitatively by non-invasive investigations. We therefore opted for an alternative strategy: to find a molecule whose levels in the blood would be associated with the functional mass of these beta cells in order to indirectly detect their alteration at the pre-diabetes stage, before the appearance of any symptoms,’ explains Pierre Maechler, a Professor in the Department of Cell Physiology and Metabolism and in the Diabetes Centre of the UNIGE Faculty of Medicine, who led this work.
Several years ago, scientists embarked on the identification of such a molecule able to detect pre-diabetes. The first step was to analyse thousands of molecules in healthy, pre-diabetic and diabetic mouse models. By combining powerful molecular biology techniques with a machine learning system (artificial intelligence), the research team was able to identify, from among thousands of molecules, the one that best reflects a loss of beta cells at the pre-diabetic stage: namely 1,5-anhydroglucitol, a small sugar, whose decrease in blood would indicate a deficit in beta cells.
© UNIGE
Encouraged by these results obtained in mice, the research team led by Pierre Maechler proceeded to the next step: determining its relevance to humans. In collaboration with numerous scientists, including teams from the HUG, they compared the levels of 1,5-anhydroglucitol in diabetic patients with those of non-diabetics. ‘We were able to observe a decrease in this sugar in diabetics. This was very motivating, especially as this decline was observable regardless their symptoms, even before the onset of diabetes’, indicates Cecilia Jiménez-Sánchez, postdoctoral fellow in the Department of Cell Physiology and Metabolism and first author of the study.
‘Diabetes is a complex disease in which many metabolic changes occur in parallel. It was therefore essential to test the relevance of this marker in people who suffer a sudden loss of their beta cells but in the absence of metabolic disorders, explains Pierre Maechler. By studying the level of 1,5-anhydroglucitol in individuals whose half of the pancreas had been surgically removed, we were able to demonstrate that 1,5-anhydroglucitol is a blood indicator of the functional quantity of pancreatic beta cells.’
This discovery opens up new avenues for the prevention of diabetes, particularly for people at risk. A simple blood sampling followed by an inexpensive specific test could identify a potential diabetes onset in these people, prompting actions to be taken before the situation becomes irreversible. ‘We still plan to test the relevance of this sugar in different types of patients and at different timescales, but it could lead to major progress in the monitoring of people at risk,’ concludes Pierre Maechler.
Source: University of Geneva
17.08.2022











