CT, PET-CT, MRT and transthoracic ultrasound in lung cancer staging
Dr Helmut Prosch, at the University Clinic for Radio-Diagnostics, Vienna, Austria, is examining the role of imaging in lung cancer diagnosis and staging. The key message of his presentation in the session EUS and EBUS vs. CT, MR and PET-CT in the staging of lung cancer is that the modalities do not compete with one another – as the title suggests – but are perfectly complimentary in the diagnostic flow.

‘In lung cancer, prognosis as well as therapy is to a large extent dependent upon tumour size at the time of diagnosis,’ Dr Prosch explains. ‘CT is the modality of choice to assess size and localisation of the primary tumour. Whether the tumour can be surgically resected is above all dependent upon the presence of metastases in the lymph nodes and within or without the chest. Surgery is indicated when only ipsilateral and hilar lymph nodes are involved and, in many cases, where ipsilateral mediastinal metastases occur after neoadjuvant chemotherapy.
‘However,’ he added, ‘if the cancer has spread to contralateral mediastinal or supraclavicular lymph nodes, a curative therapy is no longer an option.’
Non-invasive imaging is frequently inadequate to detect lymph node metastases because, in these cases, CT offers a sensitivity of only 51% and a specificity of 86%. The metabolic information PET-CT provides are a valuable complement because increased metabolic activity indicates the presence of a tumour. ‘However,’ the expert points out, ‘inflammatory processes also require more glucose. Consequently, a mere increase in glucose in the lymph nodes is no clear evidence of metastases. If the lymph nodes are large enough and negative in PET-CT we can exclude metastases with a residual probability of five percent.’
If PET-CT findings are positive, further examinations are necessary – and that is where minimally invasive procedures, such as endobronchial ultrasound, come in. In this procedure, tissue samples are taken during the examination, which means that imaging results can be supported by histological information.
Transoesophageal ultrasound is used to assess lymph nodes that cannot be reached via endobronchial ultrasound. ‘By combining these two options most lymph node metastases in the mediastinum can be well assessed and invasive methods, such as mediastinoscopy, are not necessary,’ he explains.
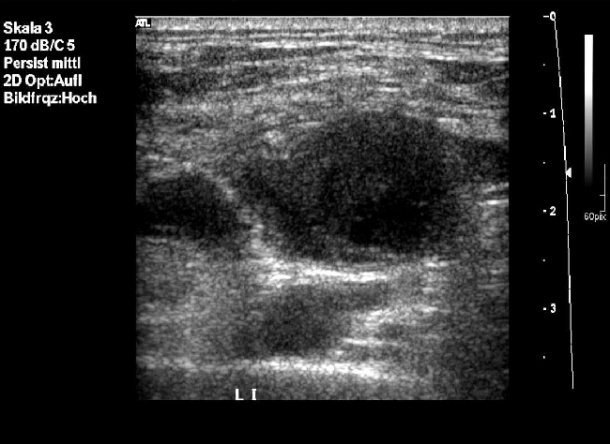
To evaluate supraclavicular lymph nodes, frequently involved in lung cancer, percutaneous ultrasound plays an important role. Dr Prosch: ‘The routine ultrasound examination of these lymph node stages offers a higher sensitivity than CT. An additional advantage is the fact that we can perform a biopsy during this procedure, which means that, with minimal intervention, we can diagnose the primary tumour at an inoperable stage.’
MRI is suited above all to brain metastases detection and the evaluation of Pancoast tumours or mediastinal infiltration.
Dr Prosch emphasises the interaction of these imaging modalities as the precondition for any meaningful diagnosis: ‘Ultrasound doesn’t compete with other modalities. Rather, it is an instrument in an orchestra and the clinician has to know when which instrument has to be played in order for the concerto to be successful.’ Thus, in many cases after initial CT scans the interdisciplinary tumour board, made up of radiologists, nuclear and internal medicine specialists and pathologists, will discuss further diagnostic steps.
EUS and EBUS vs CT, MR and PET-CT in the staging of lung cancer", Saturday, August 28, 16:00-17:30, Hall F1
Helmut Prosch
39, gained his medical degree in Vienna, Austria, and then joined the city’s Research Centre for Children with Cancer at St Anna Children’s Hospital, where his work focused on the involvement of the CNS in Langerhans cell histiocytosis.
During his later radiology training at the Institute for X-ray Diagnostics, Otto-Wagner-Spital, his supervisor was Professor Gerhard Mostbeck. Since 2010 has served as specialist registrar (Oberarzt) in general and paediatric radiology at the University Clinic for Radio-Diagnostics department in the General Hospital, Vienna.
25.08.2011