Contrast enhanced tumour studies
Medical imaging has recently advanced so rapidly that it should halt. Applying more power to computed tomography (CT) and magnetic resonance imaging (MRI) scanners is becoming too dangerous for patients and healthcare workers. Magnets for the next-generation MRIs are so powerful that they must be moved to a separate building on hospital campuses, while CT radiation levels have risen to alarming rates. Studies have also indicated a limit to diagnoses based on what we can see. Where do we go from here?
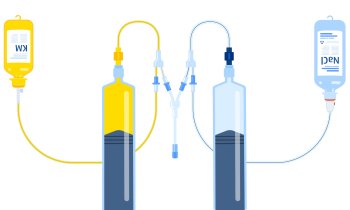
Attention is turning to the disease mechanisms that are invisible to the human eye but can be illuminated by injecting chemical agents into the blood. Even when using low-power CT, simple glucose charged with a radioactive isotope can reveal a high activity of blood flow that signals the growth of a tumour. The opposite condition, a reduction in blood flow to a known tumour site, can indicate necrosis showing that a therapy is effective in killing the tumour.
Advances in dynamic contrast-enhanced (DCE) imaging was the focus for a special session this year’s ECR, with presentations devoted to developments in CT, MRI, and the newest modality to enter this highly specialised field -- ultrasound.
Jana Votrubová MD, with Na Homolce Hospital in Prague, described techniques for DCE-CT with a focus on the unique advantages of perfusion studies of the blood-rich liver using radioactive fludeoxyglucose (FDG).
Imaging techniques make it possible for radiologists to study the entire liver, she reported, but studies have increasingly shown the emphasis on quantifying the visible changes to the tumour’s diameter and volume using widely accepted criteria for Response Evaluation Criteria In Solid Tumours (RECIST) ‘are useless’.
Instead, a study of perfusion illuminated by the FDG agent reveals more valued information about the response of a tumour to treatment.
Due to her concerns for the high levels of radiation with CT for patients undergoing serial studies of tumour response, Dr Votrubová said she is turning increasingly to diffusion-weighted imaging using MRI.
Anwar Padhani, from Mount Vernon Hospital in Middlesex, United Kingdom, presented developments in DCE-MRI, but cautioned there are limitations for this modality that challenge radiologists to ask whether they can confidently answer key questions as to whether a tumour has changed or whether a treatment is effective.
MRI does not captured an image of light but far more complex electromagnetic signals that need to be processed and can be affected by what he called ‘confounding factors’.
The drug used for the treatment might be creating phenomena revealed by MRI, such as temporary effects of increasing blood flow or arterial tension. These phenomena are assessed by software that depends upon assumptions of values. Dr Padhani encouraged colleagues to ‘know the software parameters encoded in the black box from vendors’, to be certain the defined values are appropriate with imaging objectives and the clinical questions being asked.
After the complexity and uncertain success presented by the previous speakers, there was refreshing simplicity and encouraging confidence in the description of DCE for ultrasound from Luigi Solbiati, from the Busto Arsizio General Hospital in Varese, Italy.
There is only one injected contrast agent for ultrasound, an easy to understand product called SonoVue from Bracco, with micro bubbles that suddenly illuminate blood flow when exposed to the sonic waves of ultrasound. This simple technique of physics provides a very high temporal resolution, very high spatial resolution, he reported. ‘It is fast and reliable, provides an immediate assessment and is very safe for the patient.'
It is also significantly less expensive than exams performed by the more complex CT or MRI scanners.
In fact, with a sensitivity for measuring lesions in millimetres, contrast enhanced ultrasound (CEUS) has been shown to outperform CT and CT-PET.
This quantitative measure enables the assessment of changes to a tumour following radiofrequency ablation, allowing the interventionalist to decide immediately whether to re-treat a patient while the patient is still on the operating table.
A limitation of CEUS is that the exams can only be applied to specific organs, he said, adding that a new possibility for CEUS is the delivery of therapeutics using microbubbles that can be designed to carry both a marker for a disease and a drug to treat the disease.
Acknowledging that changes to a tumour size do not always indicate the effectiveness of a chemotherapy treatment, Dr Solbiati highlighted a new pan-European study that is extracting from raw data of ultrasound signals to determine whether patients are responding to chemotherapy.
At the Radiology Society of North America (RSNA) meeting, a multi-centre study conducted in France showed how two ultrasound parameters accurately predicted after just 30 days whether a chemotherapy treatment was effective.
The significance of this conclusion, to be validated in the wider European study, is that a €200 exam can decide whether a €50,000 treatment should be stopped, continued or increased, he said.
Currently, the exam is limited to centres equipped with ultrasound scanners from Toshiba Medical Systems -- the only company to provide raw data from its signals for analysis by the French team, led by Nathalie Lassau, from the Institute Gustave Roussy in Paris.
19.04.2011