Credit: NIH
News • Oncology
Anti-inflammation approach shows promise for preventing cancer metastasis
An anti-inflammatory drug called ketorolac, given before surgery, can promote long-term survival in animal models of cancer metastasis, a team of scientists has found. Furthermore, so-called "pro-resolution" therapies can also trigger the immune system to eliminate metastatic cells. The research also suggests that flanking chemotherapy with anti-inflammatory drugs can unleash anti-tumor immunity.
The findings also provide a mechanistic explanation for the anti-metastatic effects of ketorolac, previously observed in human breast cancer surgery. Vikas P. Sukhatme, MD, ScD, dean of Emory University School of Medicine, is senior author of the paper. He was previously at Beth Israel Deaconess Medical Center and Harvard Medical School, with lead authors Dipak Panigrahy, MD and Allison Gartung, PhD. "Collectively, our findings suggest a potential paradigm shift in our approach to resectable cancers," says Sukhatme. "Clinical trials are now urgently needed to validate these animal studies."
Most cancer-related deaths come from metastases, the spread of cancer cells from a primary tumor to surrounding tissues or distant organs. The cells that seed metastases are often in microscopic clusters – a surgeon can't see them. Chemotherapy, typically given after or prior to surgery is aimed at eradicating these cancer cells in the hopes of preventing cancer recurrence. However, chemotherapy can sometimes stir up inflammation, promoting metastasis. "Cancer therapy is a double-edged sword," says Panigrahy. "Surgery and chemotherapy can induce an inflammatory or immunosuppressive injury response that promotes dormant metastatic cells to start proliferating, leading to tumor recurrence."
Ketorolac is an inexpensive NSAID (nonsteroidal anti-inflammatory drug). Because of concern over side effects, it is only approved by the FDA for short-term pain management "at the opioid level." It differs from other NSAIDs in that it preferentially inhibits the enzyme COX-1, more than COX-2. Other studies of prevention of cancer recurrence have focused on COX-2 inhibitors.
In the paper, the researchers show that preoperative, but not postoperative, ketorolac administration (as it typically is currently used), can eradicate cancer metastasis in mouse models and extend survival of animals. The effects appear to depend on COX-1 inhibition, because other NSAIDS did not display the same survival benefits. A further increase in the percentage of animals that survived following resection of the primary tumor was noted when ketorolac was combined with low dose aspirin and omega 3 fatty acids. Of note, resolvins, metabolic products of omega 3 fatty acids that accelerate the resolution of inflammation, also gave similar effects.
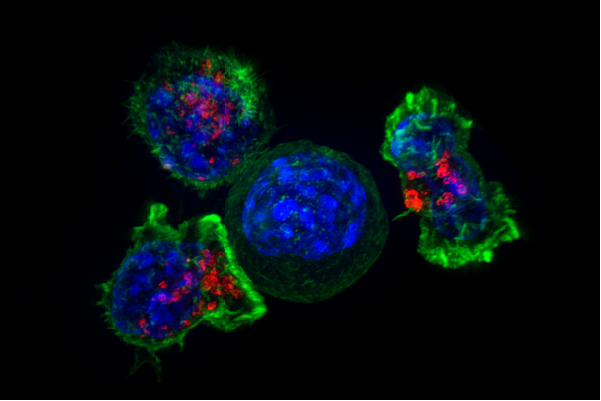
The researchers gained insight into how these approaches could be combined with other anti-cancer therapies. Ketorolac and the resolvins appear to indirectly stimulate T cells, part of the immune system, augmenting the action of immunotherapies such as checkpoint inhibitors, but conflicting with chemotherapy.
The authors conclude: "…we and others are showing that it may be possible to eradicate micrometastatic disease and dormant tumor cells without chemotherapy. Here, we demonstrate that unleashing T cell immunity by preoperative suppression of systemic inflammation or stimulation of inflammation resolution exhibits potent antitumor activity, even curing mice of micrometastases" which are largely responsible for cancer recurrence following surgery.
Source: Emory University
20.06.2019