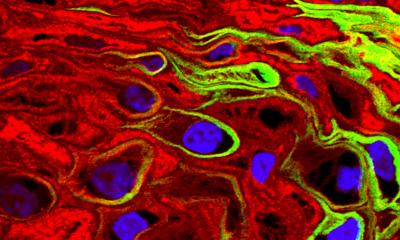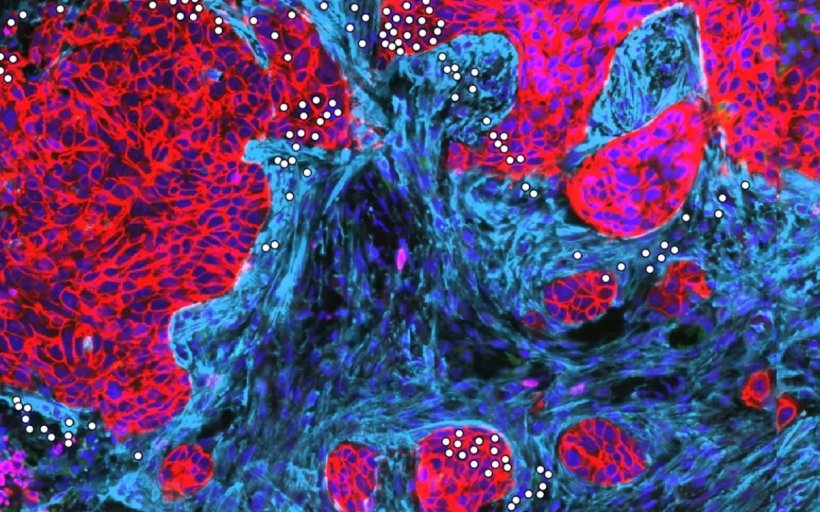
Image source: Anniina Färkkilä's research group
News • New approach to combat treatment resistance
How chemotherapy affects ovarian cancer tumours
Researchers have discovered how chemotherapy can change tumours, making them more vulnerable to new types of treatments.
These findings, which were now published in the journal Cancer Cell, could lead to personalized therapies that target the right patients at the right time, offering hope for improving care for ovarian cancer—a highly aggressive and common malignancy.
The study conducted by researchers from the University of Helsinki focused on how standard chemotherapy affects the immune system in ovarian cancer. This is a critical area of research, as current treatment options cure only a small fraction of patients. Although most ovarian cancer patients receive chemotherapy, the disease often comes back and becomes resistant to treatment.
We found that just counting immune cells isn’t enough to understand the immune system’s state. We also need to see how these cells interact with each other
Anna Vähärautio
The number of immune cells in a tumour has been shown to affect how patients respond to treatment and their overall chances of survival. However, immunotherapy, which has shown success in other cancers, has not delivered the same results in ovarian cancer. “Chemotherapy impacts the body’s immune defenses in complex ways. It can reduce the number of immune cells, but it also triggers certain immune responses and interactions that we don’t fully understand yet,” explains Assistant Professor Anniina Färkkilä, who led the study. “Our results show the importance of looking at these effects as a whole, so we can better understand how to use them to benefit patients.”
The immune system fights cancer by allowing cells to communicate and work together. This study investigated which cell types in ovarian cancer tumours interact with one another, especially after chemotherapy. Using advanced single-cell techniques, researchers were able to map the positions and interactions of individual cells in tumours with unprecedented precision. “We found that just counting immune cells isn’t enough to understand the immune system’s state. We also need to see how these cells interact with each other,” says Associate Professor Anna Vähärautio, one of the study’s lead authors.
The results showed that chemotherapy activates the patient’s own killer T-cells, which can invade the tumour and attack cancer cells. However, another type of immune cell, macrophages—sometimes called the “policemen” of cancer tissue—can block T-cells from working effectively. Macrophages do this by exhausting the T-cells and preventing them from finding and destroying cancer cells. These processes were found to increase the risk of the cancer recurrence.
The study also identified patients with very low killer T-cell activity, who could potentially benefit from therapies designed to reactivate their immune systems in the lab. “These findings will help us figure out which treatments work best for which patients and when they should be given,” says Färkkilä. “We hope this research will lead to clinical trials where patients are selected for new immunotherapy treatments based on specific biomarkers.”
The study, which analyzed nearly 120 tumour samples collected before and after chemotherapy, involved researchers from the University of Helsinki's Research Program in Systems Oncology (ONCOSYS) and the Institute for Molecular Medicine Finland (FIMM), in collaboration with the Helsinki University Hospital, the iCAN Digital Precision Cancer Medicine flagship, the DECIDER study and Harvard Medical School.
Source: University of Helsinki
11.12.2024