Obese patients in radiology - XXL challenges
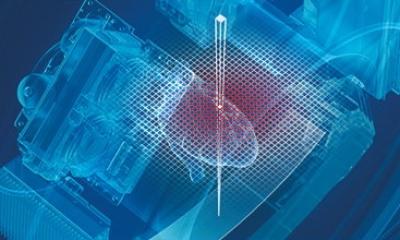
Radiological services and equipment are not yet adapted to obese patients. The accuracy of current MRI, CT and Ultrasound is hindered by subcutaneous and intraabdominal fat. These modalities are crucial in diagnosing pathologies associated with obesity, including heart-related disease. Optimising imaging modalities will be a major challenge for radiology.

The world is getting larger and sicker. Maybe not if radiology can respond to problems brought by the rampantly rising obese patient population. A manifold problem, obesity can not only generate numerous health problems, it can also hinder the imaging capacities used to diagnose those pathologies. Furthermore, it puts more of a strain on healthcare; a burden radiology could help lighten by determining primary causes earlier and diagnosing the pathologic complications of obesity more promptly. How to tackle these issues by optimising current imaging tools is the focus of the session ‘Fat radiology: Imaging in obesity and metabolic syndrome‘, presented today at the European Congress of Radiology (ECR).
Imaging capacities pushed to their limits
Obesity, long thought to be an exclusively US-localised problem, is rapidly affecting more and more individuals worldwide. In 2005 1.6 billion adults were overweight and at least 400 million were obese, according to the World Health Organisation (WHO). By 2015, 2.3 billion adults will be overweight and more than 700 million will be obese, the organisation projects. In Europe, experts estimate that at least 20% of the population are obese. In radiology, this evolution translates into a number of difficulties. First, the imaging equipment was not designed for obese patients. Tables used for computed tomography (CT), magnetic resonance imaging (MRI) or fluoroscopy examinations may not be strong enough to take the obese patient’s weight. Most CT scanners can take patients weighing up to approximately 200kg, and most MRI equipment can accommodate patients up to 160kg. For CT and MRI, the scanner‘s bore diameter may also be too narrow, with CT’s aperture diameter traditionally not exceeding 70cm, and MRI’s being even smaller at 60cm.
Rising to this challenge, vendors have responded, producing machines that overcome the limitations of current equipment, by increasing both the strength of the supporting tables and the space available for the patient. CT scanners with a 90cm wide bore and able to bear up to 300kg, and 3T MRI machines with 70cm apertures are now coming on the market, said Dr. Anthony Ryan from Waterford Regional Teaching Hospital in Waterford City, Ireland.
A challenge to imaging quality
While the cohort of obese patients stretches imaging technology to its limits, their size or `body habitus´ also compromises imaging quality. "In many cases, imaging is sub-optimal or impossible in such patients," said Dr. William Torreggiani from Tallaght Hospital in Dublin, Ireland. In particular, the abdominal region is difficult to examine with both ultrasound (US) and computed tomography (CT). Since US waves must penetrate through body tissues to produce a good diagnostic image, quality can be compromised in even slightly overweight patients, whose subcutaneous fat diminishes signal penetration. Visualisation of gall stones and other diseases linked to intra-abdominal organs may thus become significantly hindered, e.g. non alcoholic steatohepatitis (NASH), end-stage renal disease and polycystic ovaries.
In addition, moving the patient or reaching around him or her to achieve optimal imaging can be complicated. Doppler examination can be of poor quality in the obese patient and deep vein thromboses can be missed in this at-risk group. “The vendors have also responded in this regard, producing ultra-low frequency probes (down to 1MHz), in order to improve penetration and image quality” added Dr. Ryan.
In CT and MRI examinations, subcutaneous fat may also complicate organ imaging. For instance, CT local staging of colon cancer, a pathology prevalent in the obese population, may have considerably lower sensitivity. Other conditions whose detection may be hindered include coronary artery disease, prostatic, breast and endometrial carcinoma. In CT, signal-to-noise ratio is badly affected by obesity and as a result subsegmental pulmonary emboli, for example, can be missed even with increasing doses.
Finally, X-ray examinations can also be compromised by inadequate penetration and film size, interfering with the diagnosis and grading of osteoarthritis, a condition seen more frequently in the obese population. In the paediatric and adolescent population, this reduced sensitivity may make the diagnosis of Blount's disease and slipped capital femoral epiphysis more difficult. The only way to increase imaging accuracy is to augment power. While this means lowering the frequency of a transducer from currently 5-7MHz to 1MHz for US, doubling field strength from 1.5T to 3T will be necessary for MRI. Power gain in CT can be achieved by raising the kVp and the mAs. Increasing the mAs however increases the exposure to radiation.
The University Hospital of Großhadern in Munich, Germany, has recently installed the first dual source CT using two radiation sources instead of one. "Dual source CT does confer a radiation dose to obese patients, but it is probably less than conventional CT if the imaging parameters are optimised. Dual source actually reduces dose rather than increases it in most patients," said Dr. Torreggiani.
The burden on health and healthcare
Another challenge experts want to assess during the ECR session are the implications of obesity on health; an impact that radiology can help reduce. "Obesity causes more deaths each year than road traffic accidents, as a result of heart disease, peripheral vascular disease, diabetes, and cancer," said Dr. Orla Buckley from Adelaide and Meath Hospital, in Dublin, Ireland. Cardiovascular disease - mainly heart disease and stroke - is already the main cause of death worldwide, killing 17 million people each year, according to experts. "Radiology can play a role in the evaluation of patients with obesity, both in determining a primary cause and in evaluating complications of this condition," said Dr. Buckley.
Last but not least, determining risks associated with obesity has become important, considering the heavy strain the condition now places on healthcare. In Europe, obesity creates a major economic burden through loss of productivity and income, and consumes some 2–8% of overall healthcare budgets, according to a report published by the World Health Organisation Europe in 2005. "The cost of obesity on the health budget of most countries is increasing exponentially, with the indirect costs to the employer and the taxpayer remaining unquantified," said Dr. Buckley. Indirect costs include loss of earnings, loss of workforce and the cost of longer hospital stays and rehabilitation. The impact on the psychosocial wellbeing of the obese individual is immeasurable and obese people can become very isolated in society, stressed Dr. Buckley.
In 2001 the Independent UK Parliamentary National Audit Office estimated that the economic burden to the health service from obesity amounted to 2.5 billion (bn) pounds (3.3bn euros) including indirect costs, a sum it expected to rise to at least 3.5bn pounds (4.7bn euros) in less than a decade
07.03.2008