Article • Predictive plaques
Using AI for personalised prediction of heart attack
An AI-led device to assess coronary CT angiographs has been designed to assess cardiac plaque that may lead to myocardial infarction (MI).
Report: Mark Nicholls

In his presentation ‘Vascular inflammation and cardiovascular risk assessment using coronary CT angiography’ (CCTA), Charambalos Antoniades, Professor of Cardiovascular Medicine at the University of Oxford, presented the research team’s findings during the European Society of Cardiology Congress.
Speaking to Healthcare in Europe, Professor Antoniades explained that whilst heart attacks happen when plaque ruptures, blocking arteries, in around half these cases myocardial infarction is caused by a small plaque rupture. ‘However, these are plaques that have never caused any symptoms before or have been dismissed in previous angiograms as of limited importance and non-obstructive; but rupture of these minor plaques leads to the most dangerous heart attacks.’
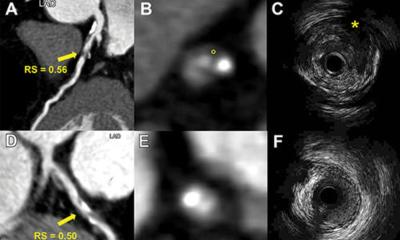
Currently, the only way to find these plaques is via standard CCTA when patients present with mild chest pain. However, even then the scan cannot show which plaques will rupture and which will not. ‘We have developed a technology called “fat attenuation indexing”, which uses artificial intelligence to analyse standard, routine coronary CT angiograms and produces a prediction about the risk of the patient having a fatal heart attack over the next eight years. By knowing who is going to have a heart attack, you know who to treat more aggressively.’
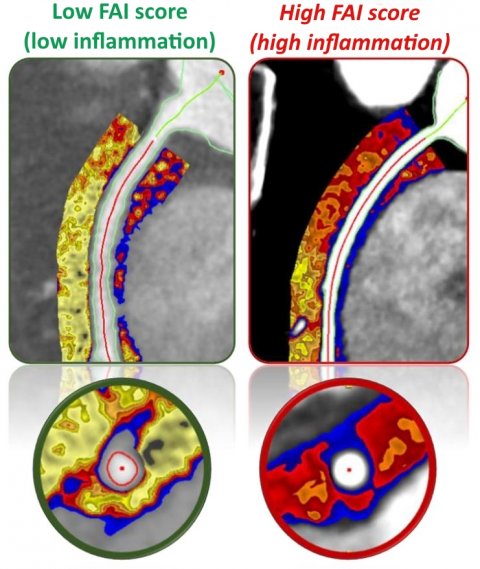
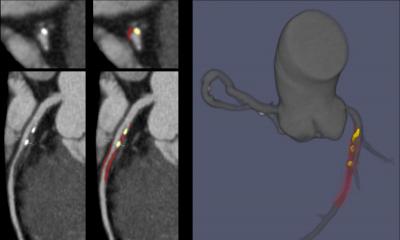
The technology works by non-invasively quantifying the degree of inflammation in the arteries from the standard coronary CT angiograms, Antoniades explained. By uploading the patient’s scan on a cloud platform, clinicians can obtain the quantification of coronary inflammation. Additionally, this medical device combines that information with the coronary atherosclerotic plaque burden and the risk factors of the patient to generate the personalised absolute risk of the patient of having a fatal heart attack, thus informing treatment decisions. ‘By knowing which arteries are inflamed,’ the professor pointed out, ‘you can predict which artery is going to develop disease in the future and also tell which artery with disease is going to give a heart attack. Then you know which is the vulnerable plaque but, most importantly, who is the vulnerable patient that needs treatment.’
Developed over the last three years, the technology has been successfully used in a research setting in large prospective trials and has already received clearance by European regulators as a medical device under the new Medical Device Regulations (CE mark). It is now used in clinical practice in hospitals.
The AI approach will advance CCTA for chest pain investigation – a first line of investigation in the United Kingdom and increasingly so in the rest of Europe and the USA. However, in up to 80% of cases, the result will still come back negative, showing no significant sign of disease and the patient is discharged. ‘The new technology analyses all cases, with or without disease, and quantifies the inflammatory burden inside the arteries,’ Antoniades said. ‘Then it tells you whether this patient who has no disease will develop the disease in the next few years, or if a patient who has had minor disease is likely to have a heart attack because that minor disease is unstable and may lead to plaque rupture in the next 2-5 years.’ By identifying patients most at risk of future heart attacks, prescribing an inflammatory agent such as colchicine – shown to be effective in preventing heart attacks – or even initiation (or escalation) of statin treatments, can be implemented.
The new medical device, called CaRi-Heart, allows clinicians to upload scans through a cloud gateway for analysis. The device then extracts information from the scans about coronary inflammation and atherosclerotic plaque burden, while it also considers existing ESC risk scoring criteria, to generate a refined, personalised absolute and relative risk of the patient for a fatal heart attack. This allows more efficient use of the ESC clinical guidelines to prevent future heart attacks in the specific population of patients who undergo coronary CT angiography. The AI algorithm for the device has a very high negative predictive value for fatal cardiac events (99.8%), and it is continuously validated and refined in a large cohort – the ORFAN study – of 100,000 patients who had CCTA and were followed up for up to 15 years. ‘In the ORFAN study, Antoniades added, ‘we are now at the stage of analysing data from all continents to project predictions in much larger populations, with representation of more ethnic groups.’
*ESC 2021 - New frontiers in cardiovascular computed tomography, August 28, 08:30am.
Profile:
Charalambos Antoniades is Professor of Cardiovascular Medicine, Director of Acute Vascular Imaging Centre and Head of the Division of Cardiovascular Medicine at the University of Oxford. His research group studies the mechanisms by which different adipose tissue depots in the human body affect vascular and myocardial redox state in atherosclerosis, using state-of-the-art non-invasive imaging techniques. He is founder of an Oxford spinout company, Caristo Diagnostics, which has developed the CaRi-Heart technology currently used in hospitals in Europe.
28.08.2021