Transcatheter aortic valve implantation
Today, transcatheter aortic valve implantation (TAVI) represents an effective therapeutic alternative to conventional aortic valve replacement for patients who are at high risk or with contraindications to surgery, and the combination of the transfemoral and transapical approaches further increases the number of patients who can be treated.

“Degenerative aortic stenosis represents a serious and growing public health problem, with regard to the demographic trends expected in the next decades. It should be addressed with appropriate resources to treat a larger number of elderly patients at high-risk or with contraindications to conventional cardiac surgery. These interventions should be less invasive than surgery, less influenced by patients’ comorbidities, and allow shorter hospital stays and faster recovery” concluded Prof Dominique Himbert from the Bichat Hospital in Paris France, at a press conference at the ESC Congress in Barcelona.
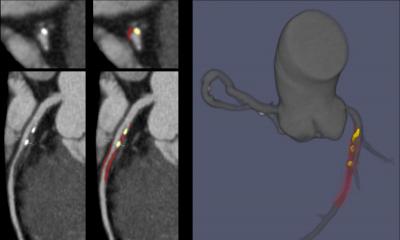
TAVI is an emerging technique offering the possibility of restoring a normal aortic valve function in patients with severe aortic stenosis, without removing the native valve, on a beating heart, without cardiopulmonary bypass and sternotomy. The prosthesis can be implanted via either a transfemoral approach, like in standard cardiac catheterization, or a transapical approach, using a direct puncture of the left ventricule.
Whatever the access used, this technique allows patients who are at very high surgical risk or with contraindications to conventional surgery to benefit from an effective treatment of aortic stenosis. A strategy integrating the transfemoral and the transapical accesses increases the number of patients who can be treated. One-year results are satisfactory in terms of survival and functional improvement, in particular given the patients’ risk profile. The most important predictor of late survival is the experience of the medical team, which underlines the necessity of proper training and the restriction of these procedures to high-volume centers.
Degenerative calcified aortic stenosis is the most frequent valve heart disease in Europe and Western countries. Its prevalence increases with age. Mild to severe aortic stenosis is present in 2 to 4% of adults over 65 years.After the onset of symptoms, average survival is 2 to 3 years with a high risk of sudden death. Surgical aortic valve replacement is the reference treatment, leading to 60 000 operations every year in the European Union. However, one third of candidates are denied surgery, particularly in the elderly, because of a perceived high operative risk due to comorbidities, or technical contraindications to surgery. Feasibility and short-term outcomes of TAVI techniques have been demonstrated in these high-risk subsets, but mid- and long-term results need to be evaluated.
The present single-centre study reports the short and mid-term outcomes of 120 patients consecutively treated by TAVI between October 2006 and June 2009. All of them suffered from a very severe and symptomatic aortic stenosis, and multidisciplinary medicosurgical consensus concluded that they had an unacceptably high operative risk or absolute contraindications to surgery.
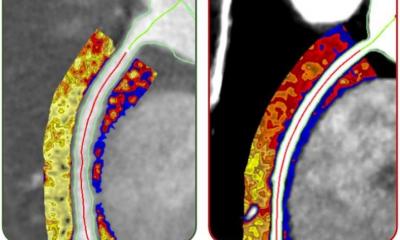
An anatomical evaluation using echocardiography, angiography and computed tomography was used to define the technical feasibility of TAVI, the approach (transfemoral or transapical) and the type of prosthesis to be used (Edwards SAPIEN THV [balloon expandable] or CoreValve Revalving System [self expandable]). On average, patients were 81 years old, more than half of them had at least 2 severe extracardiac comorbidities, and their estimated operative mortality was comprised between 16% and 27%, according to the predictive risk score used. The risk profile tended to be even more severe in the transapical group than in the transfemoral.
The prosthesis was successfully implanted in 96% of the cases. The most frequent complications were vascular (10%), due to the large diameters of the femoral sheaths, and heart blocks necessitating definitive cardiac pacing (9%). Strokes were rare (3%). Overall, procedural mortality was 3%, and 30-day mortality 9%: 8% in the transfemoral group, and 11% in the transapical group. At one year, overall survival was 79%. There was no statistically significant difference between the transfemoral (83%) and the transapical group (69%). The most important predictor of late mortality was related to the learning curve, involving the patients’ selection process, the procedural technique itself, and post-operative care. One-year survival was 60% in the first 25 patients, compared to 85% in the last 95, and this difference was statistically significant in uni- and multivariate analysis. Most important, 87% of the survivors returned to normal life, with no or only mild residual symptoms.
Today, TAVI represents an effective therapeutic alternative to conventional aortic valve replacement for patients who are at high risk or with contraindications to surgery, and the combination of the transfemoral and transapical approaches further increases the number of patients who can be treated. In the future, randomized controlled trials and comprehensive registries with longer follow-up will help to better define the safety and the durability, and subsequently, indications of the technique and the respective places of the transfemoral and transapical approaches.
01.09.2009