Surgical-site infections increase risk of blood clots
Despite receiving blood thinners and other clot prevention treatment, some patients still develop potentially lethal blood clots in the first month after their operations anyway, especially if they developed a surgical-site infection while in the hospital, according to results of a study at Johns Hopkins.
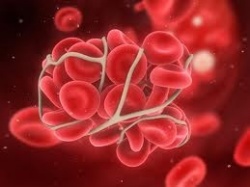
The research, described in a report published in the Journal of the American College of Surgeons, found that patients who experience a surgical-site infection after their abdominal surgery are four times more likely than infection-free patients to develop a deep-vein thrombosis (DVT) in the legs, or its more deadly cousin, a pulmonary embolism (PE) in the lungs. While only 4 percent of patients developed a DVT, 92 percent of those who did had received prophylaxis that previous research has shown is the best practice for prevention.
“We need heightened awareness about the potential for venous thromboembolism (VTE) in patients with surgical-site infections,” says study leader Susan L. Gearhart, M.D., an associate professor of surgery at the Johns Hopkins University School of Medicine. “We need to think beyond the prophylaxis we are already giving these patients. We need to think smarter.”
Nearly all surgical patients at The Johns Hopkins Hospital are routinely given proven treatments to prevent VTEs, usually the regular administration of low-dose blood thinners and the use of compression devices to keep blood flowing in the legs. Typically the treatments cease when people are discharged from the hospital.
Gearhart notes that much work in hospitals has gone into ensuring compliance with prophylaxis measures, including automated checklists to remind health care workers of their importance. VTEs are considered a form of preventable harm, and the Centers for Medicare & Medicaid Services may penalize hospitals where patients develop clots after some orthopedic procedures. But this new study shows that even when hospitals comply with prevention guidelines, VTEs can still occur.
For their study, Gearhart and her colleagues reviewed the records of 615 adults who underwent colorectal surgery at The Johns Hopkins Hospital between July 2009 and July 2011. Twenty-five (4.1 percent) developed VTE. Among patients who experienced a VTE, 92 percent had been given risk-appropriate VTE prophylaxis.
What was even more interesting to Gearhart, she says, was that 14 of the 25 patients with VTE (56 percent) also developed postoperative infections compared with 168 patients (28.5 percent) without VTE. The infectious complications in nine of the 14 patients (64.3 percent) occurred prior to or on the same day as the VTE. She says she had never before seen a link between infections and VTE in surgical patients.
One theory for the apparent link is that an increase of inflammatory protein molecules that accompanies an infection affects the functioning of platelets in the blood, which could increase the risk of thrombosis. Platelets are the sticky cells that facilitate clot formation in the blood.
Gearhart says it may be time to conduct more intense monitoring of colorectal surgery patients who develop surgical-site infections, and consider frequent screening for clots in those with infections. Such screening can be done with ultrasound equipment. She also suggests such patients be kept on blood thinners for 30 days after surgery regardless of when they are discharged.
Other Johns Hopkins researchers involved in this study include Elliott R. Haut, M.D.; Brandyn D. Lau, M.P.H.; Michael Streiff, M.D.; Elizabeth C. Wick, M.D.; and Jonathan E. Efron, M.D.
Click here for more information.
17.01.2013