Multimodality in breast diagnostics and therapy
By Professor Rüdiger Schulz-Wendtland
Early detection currently remains the most promising way to optimise the diagnosis and treatment of breast cancer, lower the mortality rate resulting from this disease, and improve patients' quality of life.

The objective is to detect breast cancers at the pre-invasive or early invasive stage where, with adequate therapy, the five-year survival rate is over 90%.
The increasing rate of pre-invasive diagnoses gives us hope with regards to a preventive contribution to lower the occurrences of the cancer. The opportunity for possible improvements of a cure through secondary prevention, at the early tumour stage, is possible with less radical and therefore less stressful therapy approaches.
The multimodal therapy concept
A multimodal therapy concept starts with an anamnesis and risk assessment, followed by breast diagnostics through clinical, sonographic, mammographic and MRI examination of the breast, as well as the clarification of suspicious results through interventional procedures – since January 2007 there has been a standard, obligatory BIRADS - clarification for all imaging procedures, which takes into account the European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis.
This is followed by the determination of the pre-therapeutic concept and then, of course, the post-therapeutic management. Multimodality or multidisciplinary care is particularly prominent in certified breast centres. From a diagnostic point of view it is very important that results from clinical examinations, mammographies, sonographies and MRI scans are centrally collated into an overall clinical picture, as this is the only way to ensure an optimum diagnosis; a strict assessment of the pros and cons of each individual examination procedure is an essential prerequisite.
Inspection and palpation (clinical examination)
Inspection and palpation are established methods of examination in clinical breast diagnostics. Although it is occasionally possible to diagnose small carcinoma
(< 1 cm, with superficial location and small breast volumes) with these methods, palpable breast cancers are often larger than 2cm at the initial diagnosis.
However, systematic clinical breast screening, by doctors or patients, has only marginally reduced the number of medium-sized tumours or the number of affected lymph nodes respectively.
Self-examination of the breast by the patient (training programme), as well as the inspection and palpation by the doctor, on the one hand have not resulted in a reduction of mortality and, on the other, have led to an increased number of biopsies because of benign (wrong positives) results.
This shows how little effect clinical examination and palpation have in the early detection.
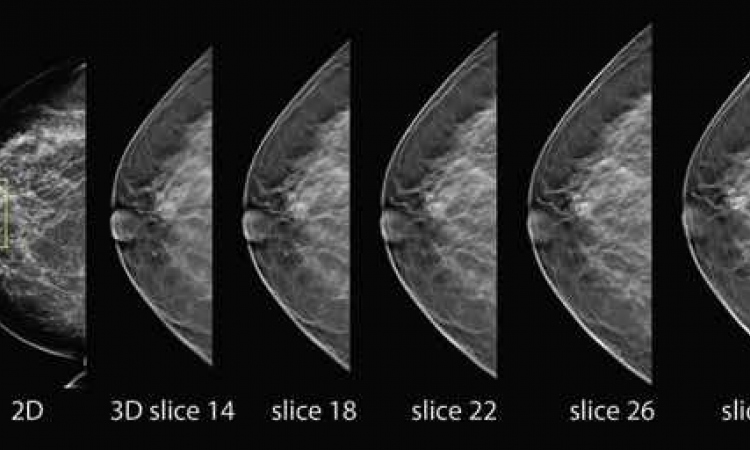
Mammography
The importance of X-ray mammography in the first instance lies in the detection of small breast cancers and the pre-invasive stages of breast cancer before they can be diagnosed through clinical symptoms. We need to emphasize that microcalcifications with a diameter of 130 µm can only be detected with mammography. No other breast diagnostic procedure delivers this scale of resolution.
The lower probability of the lymph nodes being affected with tumours smaller than 1cm clearly indicates the necessity of early detection if one takes into account that clinical screening projects have shown that in 50% of cases where the medium tumour diameter was 2cm lymph nodes metastases were already present.
The smallest breast cancers are almost exclusively detected through mammography. The accuracy of mammography for breast cancers smaller than 1cm is around 70%. The term DCIS refers to a group of histologically and prognostically heterogeneous, non-invasive breast cancers. Their detection has increased with the increasing use of mammography; the proportion of DCIS in all diagnostic malignant processes in mammography screening is up to 25%.
Microcalcifications are the primary symptom of DCIS. This is why mammography is the seminal imaging procedure – it is the only procedure that facilitates analysis of these microcalcifications. Digital mammography has now become standard and has superseded conventional film-foil mammography.
The results show equality, if not superiority, of digital mammography compared to conventional mammography, particularly for dense breast tissue, pre-perimenopausal women and women aged under 50. Digital mammography combined with CAD (computer-assisted diagnostic) systems has become so highly developed that experienced breast diagnosticians can improve their own specificity through the use of CAD for a second diagnosis. Whether digital tomosynthesis of the breast will become part of the diagnostic clarification process or whether it will develop into a procedure of primary diagnostics cannot yet be assessed.
Sonography
Breast sonography is the most important additional examination in breast diagnostics. The indications are:
• further clarification of suspicious findings following palpation
• mammographically occult clinical result
• mammographically dense mammary gland
vaccurate diagnosis of simple cysts
• additional differential diagnosis of mammographic focal findings
• silicone implants (reconstruction, augmentation)
• examination in high risk situations
• support of interventional methods
As mammography has a wrong-positive rate of 10-20%, or even up to 50%, in the detection of carcinoma, it is clear that sonography is the most important complementary procedure to mammography. Phantom examinations achieved a detection rate of more than 90% with results in the scale of 5-10mm, and this seems of particular importance for dense breast tissue. Breast sonography is carried out with a 7.5 MHz transducer; additionally the use of a high frequency transducer with 10-15 MHz is recommended.
Further opportunities for the use of breast sonography are its use in 3-D/4-D- technology, which can further improve diagnostics or, in volumetry or computer systems, which support these respectively. Whereas the additional tissue harmonic imaging (THI) procedure, which is integrated into sonography systems, has not resulted in any diagnostic improvements, it remains to be seen if this also will be the case for elastography.
In individual cases we have seen that colour Doppler sonography, with or without echo signal enhancer, can deliver additional information. If sonography can detect a mammographically hard to define node in dense tissue, and if it shows the typical features of a solid result, then this diagnosis is supported by sonography. Sonography can deliver important information for the indication or exclusion of a malignant tumour particularly in the case of mammographically dense tissue. The accuracy of sonography for the detection of malignant tumours depends on the surrounding tissue – optimum, homogenous, echo-rich tissue – as well as on the result itself, with the accuracy being limited in the case of small and in particular of pre-invasive carcinoma (DCIS).
This is why sonography must not be carried out to rule out a malignancy without mammographic correlation. Due to this limitation and the recognised dependence on examination, sonography cannot be used in the context of regular screening programmes.
Magnetic resonance imaging (MRI)
MRI is the most sensitive complementary procedure to mammography. The accuracy is dependent on technical factors, the diagnostic criteria used, as well as the patient selection. Overall MRI can achieve a sensitivity rate of significantly higher than 90%. Specificity in general is between 30 and 90%, but is highly influenced by who carries out the examination. The indications:
• DD scar/recurrence after breast cancer (<3 months post-op; < 18 months post-op including radiotherapy)
• CUP-syndrome
• high risk patient (mother and sister affected by breast cancer as well as BRCA 1 2 positive)
Further indications that have been scientifically evaluated, but are not financially covered by all medical insurers:
• Pre-operative local staging in breast cancer, in particular lobular breast cancer (DCIS-component, multifocality/multicentricity, exclusion of contralateral breast cancer),
• prosthesis/implant
• neo-adjuvant chemotherapy.
Indications show that there are new diagnostic opportunities for the diagnosis of DCIS with MRI, particularly compared to mammography. It remains to be seen whether the use of 3-T MRI systems can further increase the sensitivity and specificity of MRI in the detection of breast cancer.
07.03.2009