Article • Precision medicine
Promising radiomics for breast MRI
To develop a precise way to treat breast cancer needs standardisation and quantification of data – the only way to extract prognostic information on a large scale.
Report: Michael Krassnitzer
‘Breast cancer rates are continuously increasing, and we don’t yet have a means of prevention,’ said Dr Clemens Kaiser, from the Medical Faculty Mannheim, at Heidelberg University, who believes the only way to save more patients from death, after providing the best possible diagnostics procedures, is via precision medicine: the right treatment at the earliest possible time. The radiologist spoke of the implementation of precision medicine for breast cancer during a Siemens Healthineers satellite symposium held at the 2018 European Radiology Congress in Vienna.
Strong prognostic tool

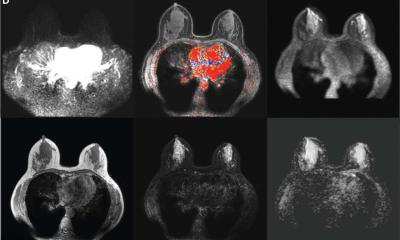
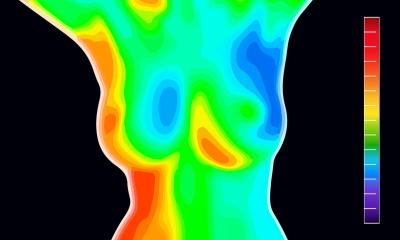
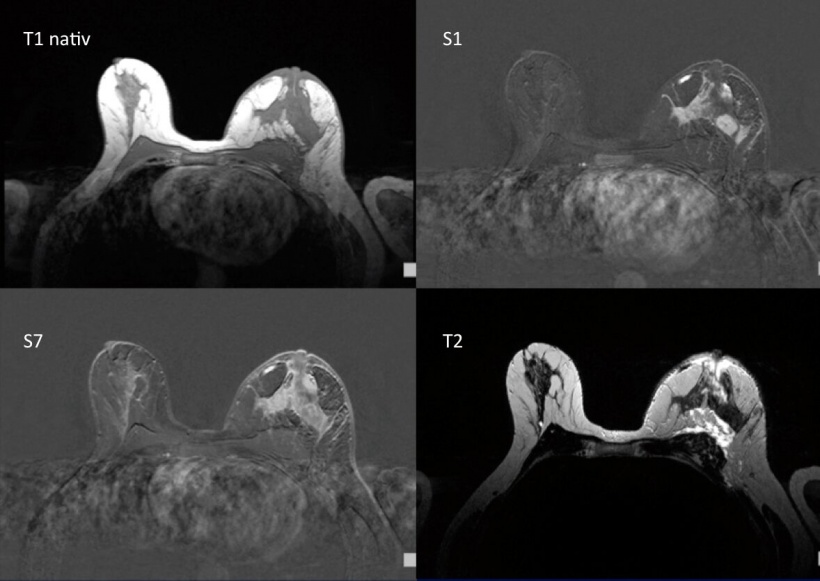
In Kaiser’s view, the key to precision medicine in breast cancer treatment is MRI: ‘Breast MRI images deliver a lot of prognostic information,’ he confirmed. Studies have shown that breast MRI data allows conclusions as to the risk of metastases. Other studies have shown a link between breast MRI data and chances of survival. ‘Breast MRI is a strong, non-invasive prognostic tool,’ Kaiser confirmed. The inner structure, or margin of the tumour, oedema, the hook sign (a tumour branch) or necrosis – all of these can contain important information that can be decisive for treatment.
The problem is that automatic quantification of all these factors and ability to derive prognoses from them is not yet possible. ‘However, the prerequisites are there,’ Kaiser emphasised. The amount of medical data available is escalating – keyword: big data. Whilst in 1980 it still took seven years for the entire volume of available medical data to double, this now takes only a year. It is estimated that by 2020 it will only take 73 days. The capability of computers has also increased in line with the level required for these tasks – a modern mobile telephone is 32,000 times faster than the best computers available at the time of the moon landings.
Data quantification
This would be an opportunity to obtain comparable and valid data that could deliver prognostic information via radiomics
Clemens Kaiser
‘Radiomics’ might be the solution. The word describes a combination of medical image processing and radiological research into the analysis of quantitative image characteristics in large, medical image databases. This is based on the idea of being able to make statistical statements about tissue characteristics, diagnoses and the course of diseases using radiological imaging data, which could otherwise only be achieved through genomics or proteomics – i.e. exactly what Kaiser is envisaging with regards to breast MRI. ‘We must,’ he said, ‘extract as much prognostic information from breast MRI images as possible.’
This is also not as easy as it sounds. The automated evaluation of image databases still faces obstacles. A very essential one is the lack of standardised data: ‘Standardisation is the big challenge,’ the radiologist emphasised. As long as the data is not standardised because each facility and institute carry out investigations in their own individual way, it cannot automatically be combed through for information. ‘We must quantify the data,’ Kaiser stressed. How might that be achieved? Kaiser envisions a simple, solid decision tree, such as the one published by radiologists at the Medical University of Vienna around four years ago to differentiate between benign and malignant lesions in breast MRI. ‘This tool has a proven accuracy of 88% for the distinction between benign and malignant tumours and helps to achieve a definitive diagnosis for a third of all lesions.’
If examinations were always carried out based on these decision trees this would result not only in a consistently improved precision and standardisation of a diagnosis but also in quantified examination data. ‘This,’ he believes, ‘would be an opportunity to obtain comparable and valid data that could deliver prognostic information via radiomics.’
Profile:
Radiologist Clemens Kaiser MD BA is a Senior Consultant and Head of the Division for Multimodal Breast Diagnostics at the Institute for Clinical Radiology and Nuclear Medicine, University Hospital Mannheim, Germany. He held his International Business Administration (EMA) diploma and Bachelor of Arts in Marketing Management, before gaining a PhD in medicine at the Friedrich-Schiller Univer-sity Jena. His dissertation was entitled ‘Duct-obstruction-sign – duct ectasia for differential diagnosis of DCIS vs papilloma in breast MRI’.
07.05.2018