Interview • Big Data
Automation helps radiologists
The billions of medical images taken and diagnoses made every year across the globe are as varied in quality, detail and structure as the situations in which they are obtained.
Interview: Sascha Keutel
Contrary to popular belief the huge majority of medical data is available only in unstructured form which considerably impairs efficiency in the healthcare system. Peter Aulbach, Siemens Healthineers’ Business Manager for CT in Germany, explains how these data – if they were analysed systematically – could provide clinical insights and help improve patient care.
Many research projects worldwide focus on machine learning: software that is able to automatically answer clinical questions such as the assessment of medical images. How will such algorithms impact the healthcare system?
That is a very exciting field of research which will dramatically alter the healthcare landscape. As a company we are observing a few trends that are most likely here to stay, such as automation, you mentioned it, or the increasing role of artificial intelligence – AI – in healthcare. All these topics aim to generate many and above all comparable, respectively reproducible data.
In which areas will artificial intelligence play a role?
AI is primarily important in decision support systems. We talk about artificial intelligence when an algorithm or a software programme can learn and suggest a diagnosis or even a therapy based on evidence. The more the system learns the better it will be in the future and the fewer user interactions are required.
That is a prospect many people find scary.
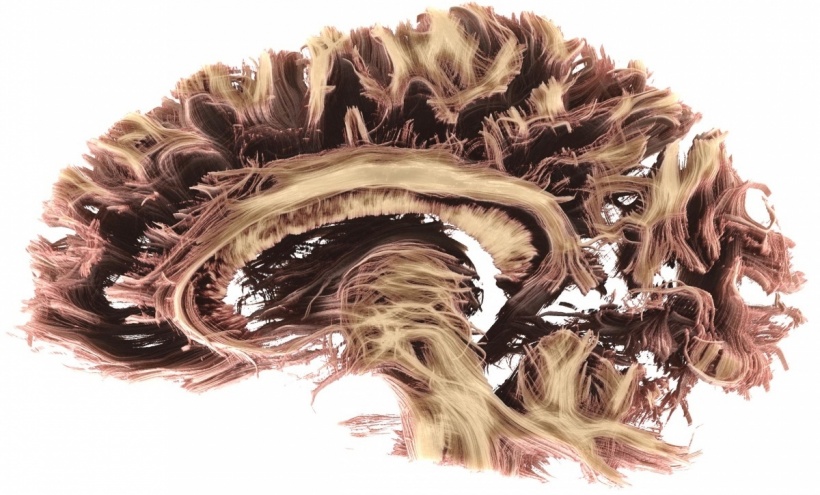
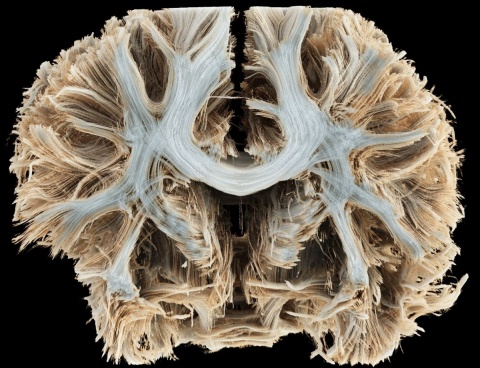
Maybe. One thing, though, is certain: We cannot work without computers anymore! Computers are far superior to human beings when it comes to rational intelligence and they do make better decisions. That’s a fact. Ideally, we manage to align the machine‘s rational intelligence with the emotional skills that characterize us as human beings. The population is ageing and we need more and more trained people who are able to diagnose, interpret and treat. But the number of these people does not increase exponentially; quite on the contrary, the number of experts is decreasing, widening the gap in our system. That also holds true for radiologists who are inundated with slice images and are having an increasingly hard time catching up. With DNA sequencing, functional MRI and CI imaging and many other digital developments, the data floods will continue to rise.
This is where radiology is facing another problem: We still lack standardisation and structured storing of image and diagnostic data. Amassing data won’t help if these data are not structured. Huge unstructured data pools are useless. Today, most of the data obtained gather dust so to speak in the modalities; only 2 percent are archived for later use.

What would a solution look like?
We consider so-called DICOM structured reports to be key. These reports are the wheel-barrows with which data are carried from the modality to a Big Data form. Widely used structured reporting will ensure that quantified data are transferred automatically from the imaging modalities to the PACS – and thus are converted into a Big Data-usable form.
In the USA, for example, by law every TV show has to be transformed into text. The texts can be analysed using algorithms. Thus you can find out how often the words Clinton or Trump or any other word were used in a certain period of time. That’s a quintessential Big Data application.
In our field, however, things are much more complicated. While we do have many video and image data, they are of little value since they are not categorised. The structured report is the key to this treasure trove. Templates will allow us to make huge steps forward, since templates are configurable, but even more importantly – if DICOM and HL7 can agree on a single standard – they will contain the acquired image data as well as the AHA and ACC guidelines and transfer these templates to the PACS.
You aim to automate sequences, protocols and post-processing. Won’t that make the radiologist obsolete?
No, we don’t want to make the radiologist obsolete. Quite on the contrary: we want to make all data available which the medical expert needs to get a full picture of the situation. Going forward, the radiologist will be an information broker who leverages the modalities, which are high performance systems generating reproducible results, with little standard deviation and in a structured way. He no longer will have to sit in front of a screen and plough through reams of slices to arrive at a conclusion.
This is where radiomics comes in. In the US, there is a company with this name that owns a patent on the analysis of oncological image data from MRI and CT scanners and already offers pattern recognition.
25.11.2016











