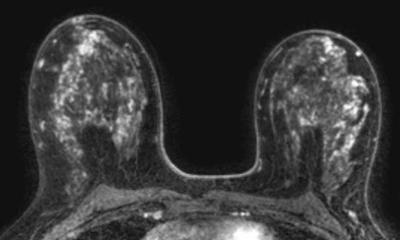
Pre-operative breast MRI
Report: Mark Nicholls
Performing pre-operative breast MRI in all women with invasive lobular carcinoma (ILC) can reduce the need for re-excision, according to a study conducted through two major cancer centres - the Radboud University Nijmegen Medical Centre and the Netherlands Cancer Hospital/Antoni van Leeuwenhoek Hospital.


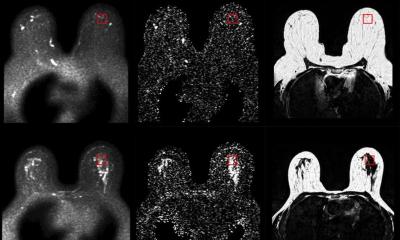
The study’s coordinator Dr Ritse Mann (Dept. of Radiology, Radboud University) said: ‘We investigated whether the performance of pre-operative breast MRI in women with ILC -- approximately 15% -- would be beneficial for these women in terms of outcome. It has been clearly demonstrated that the performance of pre-operative MRI, if adequately conducted and analysed, does improve the estimation of tumour extent. It was, however, uncertain whether this better delineation could be translated to better surgery.’
In a project that involved close cooperation between the departments of radiology, surgery and pathology, the researchers stratified patients with ILC into a group of patients who underwent pre-operative MRI and a group of patients who only underwent mammography and ultrasound in the pre-operative evaluation. ‘Subsequently we assessed the rate of re-excisions, the rate of mastectomies and the time to final surgical therapy in these groups,’ he said. ‘Our study shows that, in experienced hands, the knowledge of breast MRIs can be successfully transported to the operating room and be effectively used to reduce the rate of unsuccessful operations, especially in the difficult cases that ILC usually present.
The rate of tumour positive margins that re-excision was indicated for dropped dramatically from 27% to 9%, without an increase in the rate of mastectomies.
‘Moreover, while the need for re-excision almost doubled the time to complete surgical therapy, pre-operative MRI can be performed easily in the waiting time for surgery.’
He added that the study findings were significant because it showed the performance of a simple diagnostic test – a 15-minute breast MRI scan - may save many women from unnecessary secondary surgery.
In The Netherlands, more than half of university hospitals and major teaching hospitals now perform breast MRI. ‘In Europe, breast MRI is becoming a well-accepted clinical modality. The Eusobi guidelines for the performance of pre-operative breast MRI endorse the use of pre-operative MRI in all patients with invasive breast cancer, though currently only for screening of the contra-lateral breast.
‘The fact that we can show that it is also good for evaluating the primary tumour is only strengthening this advice.’
Among clear benefits for patients: they are less likely to require secondary surgery after an initially failed attempt to excise the tumour radically. ‘This reduces anxiety, improves the cosmetic outcome and reduces time to final surgical therapy. They do not need to worry about unnecessary mastectomies, as the knowledge from the MRI can actually be used to better delineate the tumour and hence perform an adequate lumpectomy. Findings that will change the therapy to mastectomy should be biopsied first,’ he added.
For clinicians, pre-operative breast MRI means the multidisciplinary team has a clearer idea of the tumour they are treating and can adapt their therapeutic plan to the actual tumour characteristics. ‘Early indications are that this technique is cost-effective as it results in a decrease in the rate of re-excisions and less operating theatre time is necessary, which might decrease waiting times for surgery.’
While no cost-analyses have been performed, in the Netherlands a breast MRI costs around €300, while surgery amounts to €5000.
Dr Mann stressed that it is essential to understand that working with breast MRI is substantially different from mammography. ‘Rather than the conventional 2-D approach from mammography, breast MRI is truly 3-D and needs to be appreciated in this way. This is a challenge for both radiologists and surgeons alike.’
The next step is to investigate whether pre-operative MRI also has an effect on long-term outcomes, such as recurrence and survival, and whether the results can be extrapolated to patients with other types of tumour.
17.05.2010