PET/MR: The opportunities are almost unlimited
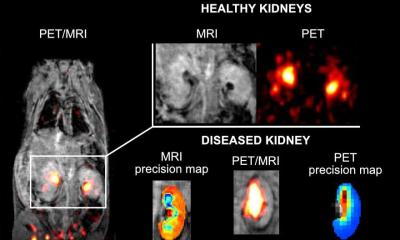
MRI has become the gold standard for many indications in cardiac imaging, apart from imaging the coronary arteries. For function and morphology assessment, MRI is the leading technology. A further advance into as yet unknown territory is myocardial imaging aided by one of the first integrated 3-Tesla PET/MR systems currently used at the Institute of Radiology, Essen University Hospital, Germany.
Report: Daniela Zimmermann


Last year, the Essen team published the world’s first case report on PET/ MR cardiac imaging in the renowned journal Heart. Opportunities for cardiovascular imaging are nowhere near being fully known and explored, enthused Felix Nensa, a member of Essen’s Cardiovascular Imaging Working Group. ‘MRI has the advantage that it lets us assess the individual anatomic compartments and different soft tissues much better than CT. The heart is not simply positioned in an axial transverse but in a quite complex position in the body. With the help of localisers, we position the MRI scanner along the anatomic axis, rather than the body axis, and we can also determine many different axes, planes and contrasts,’ he said, explaining some MRI advantages over CT. An MRI examination initially starts with a standard protocol that provides an overview over the heart and surrounding areas. This is followed by different, specific heart protocols, and often includes an assessment of the heart function, i.e. moving heart imaging.
Myocardial Infarction: How T-2 weighted sequences and late enhancement can provide information on the point in time when an infarction occurred ‘If the heart function measurements, such as 3-D volume reconstruction or four-chamber view, result in conspicuous findings we perform further diagnostic evaluations with T-2 weighted sequences. As fat is suppressed in these examinations and water becomes more visible, this is a particularly good way of visualising oedema within the myocardial wall (tissue classification). Increased build-up of water in the tissue is clear evidence of an acute infarction or inflammatory heart disease.’ Myocardial blood-flow is assessed with a dynamic contrast-enhanced perfusion examination.
This is followed by one of the most important sequences of the cardiac examination: Around ten minutes after the perfusion with contrast media, it is possible to detect the so-called late enhancement – bright areas that result from the contrast media accumulating in certain parts of the myocardium. This is clear evidence of perished myocardial tissue, which could have been caused by an acute infarction or a chronic scar. ‘This sequence is incredibly sensitive and anatomically of a very high resolution, therefore also making very small scars in the myocardium visible. But we can only determine how long the tissue has been dead by assessing it in combination with the T-2 sequence. Only once an oedema is also visible in late enhancement can we be sure that it is an acute infarction; however, if no oedema is visible in this location it is an older scar, Felix Nensa explained. This is important because it impacts the treatment and the chance of a cure.
Tricking cardiac metabolism with glucose
Many of the examinations described can also be carried out with procedures used in nuclear medicine; in this context, PET images have a significantly higher resolution than, for instance, those from myocardial scintigraphy. The basis of PET scanning is the imaging of the metabolism, which is also utilised for PET/MR scanning: Under normal circumstances the heart specifically metabolises fatty acids; however, if it is exposed to a real ‘glucose shock’, with the patient taking 75 grams of glucose, the heart changes its metabolism to sugar. ‘This is helpful to assess infarctions. In a healthy patient, the radio-labelled glucose ‘glows’ homogenously in the left ventricle; if it doesn’t, then this indicates a type of pathology. The lack of glucose metabolism is an indication of dead tissue,’ he pointed out. However, there are other situations – for example, where the myocardial tissue is still intact, but no sugar or only a little sugar is being metabolised, as is the case with the so-called ‘stunned myocardium’.
If it was possible to open the coronary artery very soon after an infarction occurred the damaged tissue in this area might recover, which is why an oedema is normally visible on the MRI scan but no late enhancement, because the tissue has not died yet. In those cases the PET scan provides complementary information that might help to further assess the state of the jeopardised myocardium. There are also cases where the left ventricle ‘glows’ very intensively. This can be an indication of a ‘hibernating myocardium’, characterised by chronic under-perfusion. The MRI scan shows that this area is less perfused, which may point towards a problem with heart wall motion. ‘One assumes that the tissue acts auto-protectively and that a stimulus sends signals to the heart tissue to use as little oxygen as possible to stop it from dying.
Normally one would also expect that less glucose is used in this area, but the opposite is actually the case. Unlike beta-oxidation during the fatty acid metabolism, anaerobic glycolysis requires almost no oxygen during the glucose metabolism. Although researchers don’t yet agree, one possible explanation may be that the myocardium switches to the lowest-impact metabolic procedure when there is little oxygen available. Assessment of vitality in under-perfused tissue is also particularly important for planning of further treatment because revascularisation of obstructed coronary arteries only makes sense if the tissue has not yet completely died, Dr Nensa explained.
Tracers as keys for metabolic information
With PET/MR, excellent anatomic resolution is combined with the metabolic information delivered by the PET. The most established tracer for the myocardium is 18FFDG, a radio-labelled glucose. For myocardial perfusion examinations radio-labelled ammoniac (13N-NH3) is commonly used. These two tracers are also the basis of purely nuclear medical PET examinations without MRI, as only the combination of the two tracers allows for a safe diagnosis. In Europe, radio-labelled water and rubidium are less established tracers for perfusion. Rubidium has the advantage that it can be manufactured with a generator on site while its half-life is only 90 seconds. Perfusion assessment with classical MRI contrast agents suffer from contrast agents entering the intercellular spaces and remaining there for some time – an effect that is very welcome for late-enhancement but less so for perfusion, as it makes the conversion into absolute flow rate very difficult.
‘In the case of a patient with three-vessel disease we are then missing the point of reference. Water, which can freely diffuse, is ideal for perfusion. However, not all tracers can be combined in one examination because they all emit the same radiation of 511 keV. When several tracers are to be combined, such as 18F-FDG with a perfusion tracer, the nuclear team carries out an overlay, meaning that an image with a certain tracer and a certain intensity is over-framed by a tracer with a markedly higher intensity.
On the trail of cardiac insufficiency
Further, very promising tracers are C-11-hydroxyephedrine (11CHED) and iodine-marked MIBG (124l-MIBG), which act as a nor-/ adrenaline analogues, taking the neurotransmitter’s place, i.e. in the heart’s sympathetic nervous system. With these tracers the regrowth of synaptic connections between the heart and the nervous system can be verified in patients with heart transplants. A further important area of application for nor-/adrenaline analogues is cardiac insufficiency. As more and more people survive cardiac infarctions these days there is an increasing number of patients with heart failure because of reduced cardiac output due to areas of myocardial scarring. Left ventricular ejection fraction, which is reduced in the case of cardiac insufficiency, is an important parameter for the assessment of cardiac performance. ‘The big advantage of PET/MR is the fact that it not only allows us to determine the left ventricular ejection fraction but also the sympathetic innervation, which is usually also compromised. We can now visualise this with the PET/MR,’ the radiologist explained. 123l-MIBG has been used for single-photon emission computed tomography (SPECT) for some time, although so far without good anatomic reference –which is now possible through PET/MR.
Inflammatory changes and tumorous diseases
In future, PET/MR scanning is also likely to play an important role in the diagnosis of cardiac inflammatory changes and tumorous diseases. Myocarditis, an inflammatory disease affecting the myocardium and most often found in young people as a result of protracted flu, is very dangerous. So far, inflammation of the myocardium has only been possible to confirm via biopsy, which, although highly specific, is not particularly sensitive, meaning that an inflammation can only be pathologically confirmed if the tissue has been sampled in exactly the right location. If the myocardium is completely switched to fatty acid metabolism, therefore becoming ‘silent’ for the 18F-FDG tracer, it is possible to confirm that there is an inflammation in those places where glucose accumulates, as inflammatory cells are not capable of a fatty acid metabolism and only able to perform glucose metabolism. This means that an 18F-FDG scan after one day of Atkins diet makes it possible to distinguish between inflammatory cells and normal cells. The same applies to tumorous diseases of the heart. Tumour cells also metabolise sugar to a great extent. This even makes it possible to distinguish between benign and malignant tumours. It also enables detection and treatment of diseases that are hard to diagnose, such as cardiac sarcoidosis, at an early stage. ‘It’s specifically the combination of both procedures that is so promising and where there are almost unlimited opportunities for cardiovascular imaging,’ he noted.
Essen benefits from good interdisciplinary co-operation, along with input from siemens Presently, the Essen team is entering considerable uncharted territory and the relevance of their results is not always obvious and clear. However, in many cases, the response to certain treatments can already be assessed with more ease. Essen’s traditionally close cooperation between radiology and nuclear medicine on the one hand and device manufacturer Siemens on the other hand greatly facilitates the clinical evaluation of that complex technology. ‘We’ve come a long way and are now in the process of implementing the first, concrete studies,’ Nensa revealed. Only with clear clinical indications the project PET/MR will become truly established and economically viable. As a reference centre for Siemens the Essen team are among the first to clinically evaluate newly developed technology. On the other hand, Siemens are also happy to listen to experiences and suggestions from Nensa and his colleagues. ‘This exchange is extremely important for both sides; it’s give and take – we have the very latest technology at our disposal and deliver the latest findings about it. Both sides have the same objective: to advance technology even further to ultimately improve patient care,’ the radiologist is happy to report.
PROFILE
Directly after completing his final school exams, Felix Nensa freelanced as a software developer for the Research Institute for the Diagnosis and Treatment of Early Lung Cancer at the Augusta Hospital in Bochum, where one of his projects included programming new diagnostic software for automated sputum cytometry. At that time he also took a distance learning degree course in IT (2000). His medical studies at Ruhr University in Bochum (2001-2007) included two semesters spent at the University of Strasbourg in France. During this period he continued work at the Augusta Institute and, in 2008, began his dissertation – Comparison of spirometry and body plethysmography as detection methods for bronchial constriction in an unspecific provocation test with methacholine. In 2011, Nensa became a registrar at the Institute for Diagnostic and Interventional Radiology and Neuroradiology at Essen University Hospital and manages research projects on PET/MR, Cardio-MRI and DCEMRI
08.03.2013