Novel diagnostic strategies and the future of breast cancer care
Karoline Laarmann reports
During his Honorary Lecture at the 8th Düsseldorf Breast Cancer Conference in Germany world renowned surgeon and oncologist Prof. Veronesi reflected about the prevention and treatment of breast cancer.
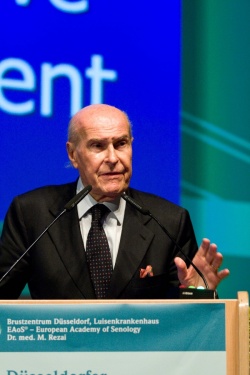
With a medical career spanning 50 years, 85-year-old Italian surgeon and oncologist Professor Umberto Veronesi, Founder (in 1994) and Scientific Director of the European Institute of Oncology in Milan and former National Health Minister (2000 – 2001), is internationally recognised for his contributions to breast cancer prevention (e.g. studies on tamoxifen and retinoids) and treatment; breast-conserving surgery having invented quadrantectomy; improvement to sentinel lymph node biopsy, and making the avoidance of axillary dissection possible in breast cancer with clinically negative lymph nodes.
During his Honorary Lecture at the 8th Düsseldorf Breast Cancer Conference in Germany Prof. Veronesi reflected: ‘Surgery of breast cancer, more than in other tumours, has gone through a number of revolutions in the last forty years, which did not so much manifest in techniques but in concepts: The rethinking from anatomical concept of cancer spread to biological concept, as well as the paradigm shift from maximum tolerable treatment to minimum effective treatment, are two milestones to mention.’
Both more patient-friendly concepts were essentially initiated by the professor himself in his Milan Trials I – IV. He was the first to prove in a clinical trial published in 1981 that patients with small-size breast tumours undergoing a quadrantectomy (quadrant resection flanked by radiotherapy and axillary dissection) have the same recovery chances as patients undergoing radical mastectomy. The results also revealed that breast cancer is a systemic disease, instead of a local disease as believed in earlier doctrine, which means that metastases spread from early on in the periphery. Consequently local recurrence is not an instigator of new metastases and the survival rate of lumpectomy + radiotherapy and quadrantectomy + radiotherapy is the same.
A discussion raised by the introduction of conservative breast surgery was the evaluation of margins of resection as a possible predictor of recurrence. ‘Our Milan trials have shown that patients with negative or positive margins have the same rate of recurrence’, Prof. Veronesi. ‘The evaluation of the margins is limited, first because the peritumoural spread of cancer cells is often discontinuous and, second, the biopsies on the margins of the specimen are “at random”. After surgery, we believe that some cancer cells remain in the breast and therefore radiotherapy must be given to all patients following conservative surgery.’
In the ’90s, the professor began to perform sentinel node biopsy as a method for screening the axillary nodes for metastasis in order to spare healthy axillary nodes. The sentinel node is the first that receives lymph from the tumour area, so only if the sentinel node is afflicted by cancerous cells, should all lymph nodes be removed, he said. Another powerful prognostic indicator is the internal mammary node. ‘Mammary internal nodes are generally ignored by surgeons, but my clinical experience shows me that if axillary nodes and internal mammary nodes are both negative, survival is good; if they are both positive, survival is bad, and if only one of the two is positive the prognostic power is identical. In other words, the identification of the internal mammary node has the same prognostic value as the identification of the axillary node. Hence, patients with positive internal mammary nodes should receive radiotherapy to the internal mammary chain and more intense systemic treatment.’
The further step to improve breast conservation was the development by Prof. Veronesi of ELIOT (Full Dose Intra-operative Radiotherapy with Electrons). ELIOT is a focalised therapy technique to treat a more limited volume of tissue surrounding the tumour bed. A mobile linear accelerator is utilised to deliver a single dose of radiation (50 Gy in three minutes) with multi-energy electrons immediately after the removal of the primary carcinoma. ‘The concept behind ELIOT is that local recurrences occur in 90 % of cases in the quadrant harbouring the primary breast carcinoma. So with ELIOT, we are able to pin-point the irradiation on the operative field. A dedicated disk of lead and aluminium is used as a protective device. Therefore, ELIOT reduces radiation exposure to the normal tissue as well as to deep organs like the lung.’ Because the radiation course is shortened from 5-6 weeks to only one session, the problem of access to radiotherapy centres, especially in rural areas, is also solved.
Summing up, Prof. Veronesi presented his list of the most important, novel, targeted minimally invasive treatments:
- High-Intensity Focused Ultrasound (HIFU). This uses high frequency sound waves to heat up small accurately-targeted amounts of tissue to a temperature of 80-90◦C. The main advantage of ultrasound in radiotherapy is the real-time guidance without the need of surgical exposure or insertion of instruments into the lesion.
- Proton Beam Therapy (PBT). The energy that protons deliver to the tumour mass is much higher than the usual electron photon beams. While the latter go through the whole body, the irradiation with protons can be controlled to stop, when it has reached the target tissue and to unfold its complete power in the tumour volume first.
- Intra-operative Avidination for Radionuclide Therapy (IART). This is a complex, two-step procedure consists. First the exogenous molecule Avidin is injected in to and around the tumour bed during surgery. Next, the day after, radioactive biotin is intravenously injected into the tumour area. Because Biotin shows a high affinity to Avidin, the intra-operative treatment with Avidin allows for a fast and stable uptake of the radionuclides into the tumour cells.
- Endocrine and biomolecular treatments, like drugs targeting the HER2 receptor, which follow a ‘target and control’ instead of a ‘search and destroy’ strategy in cancer. These tumour-biological therapies enable increasingly tailor-made, individualised treatment for the patient.
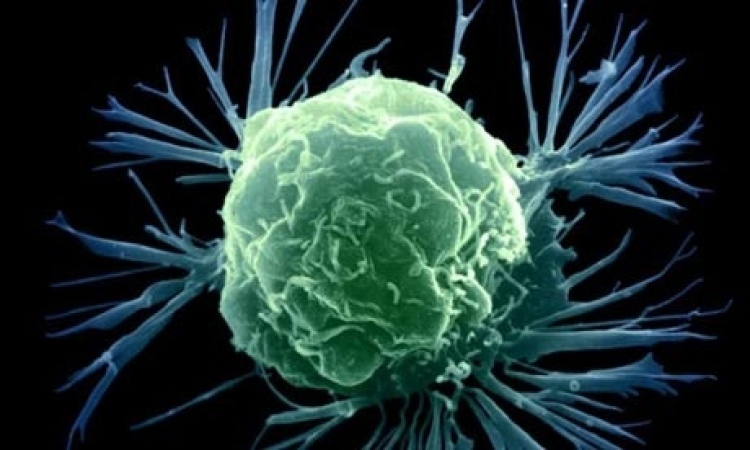
- The concept of cancer stem cells as the ‘root’ of a tumour: ‘Recent finding suggest that at the heart of every tumour lie a handful of malignant stem cells able to maintain the malignant tissue. In vitro and animal models have demonstrated that breast cancer stem cells are relatively resistant to both radiation and chemotherapy. We need to change our policy of treatment and try to identify markers and membrane receptors of these cancer stem cells as targets for new drugs. For surgeons, knowledge about the presence or absence of cancer stem cells in a sentinel node biopsy could be of great help in decision-making if dissection of sentinel node is needed or not.’
07.09.2010