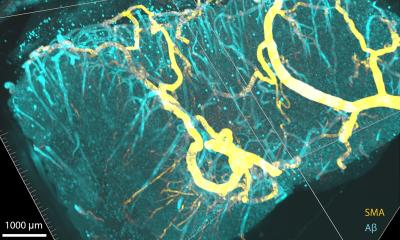
Image source: Ozturk et al., 2020, Science Advances (CC BY-NC 4.0)
News • Glioblastoma
New imaging technique to study 3D printed brain tumors
Glioblastomas are complex, fast-growing malignant brain tumors that are made up of various types of cells. Even with aggressive treatment — which often includes surgery, radiation, and chemotherapy — glioblastomas are difficult to treat, leading to an average survival of 11-15 months.
In research published in Science Advances, Xavier Intes, a professor of biomedical engineering at Rensselaer, joined a multidisciplinary team from Northeastern University and the Icahn School of Medicine at Mount Sinai to demonstrate a methodology that combines the bioprinting and imaging of glioblastoma cells in a cost-effective way that more closely models what happens inside the human body.
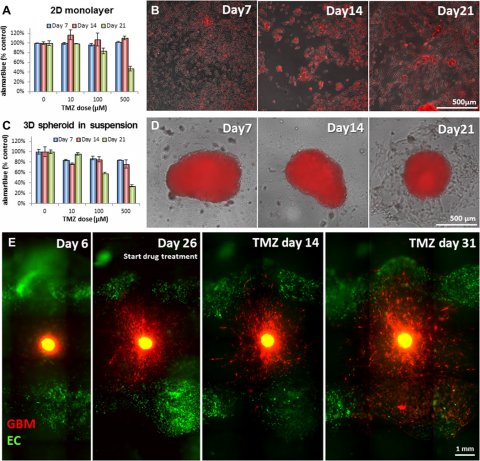
Image source: Ozturk et al., 2020, Science Advances (CC BY-NC 4.0)
“There is a need to understand the biology and the complexity of the glioblastoma,” said Intes, who is also the co-director of the Center for Modeling, Simulation and Imaging for Medicine (CeMSIM) at Rensselaer. “What’s known is that glioblastomas are very complex in terms of their makeup, and this can differ from patient to patient.”
To create their 3D tumor cell model, a team, led by Guohao Dai, an associate professor of bioengineering at Northeastern University, made bioinks out of patient-derived tumor cells and printed them along with blood vessels. That vasculature allowed the printed tissue to live and mature, enabling researchers to study it over a matter of months.
The bioprinted blood vessels also provided channels for therapeutics to travel through — in this case, the chemotherapy drug Temozolomide. In the body, drug delivery to glioblastoma cells is especially complicated because of the blood-brain barrier, a wall of cells that blocks most substances from reaching the brain. Because it can more closely replicate this impediment, the team’s method provides a more accurate evaluation of a drug’s effectiveness than directly injecting the therapy into the cells. “That’s the unique part of the bioprinting that has been very powerful,” Intes said. “It’s closer to what would happen in vivo.”
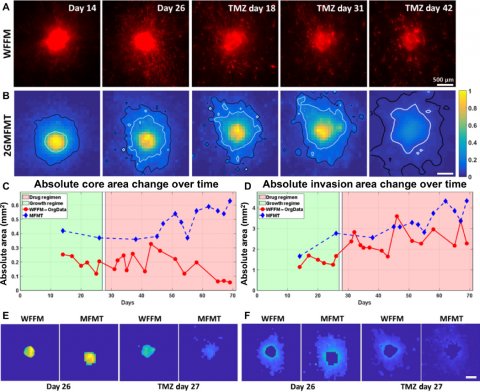
Image source: Ozturk et al., 2020, Science Advances (CC BY-NC 4.0)
In order to see if the therapeutic was making it to the glioblastoma cells and working, Intes and his team developed a specialized technique that could quickly take images of the bioprinted tissue at the cellular level through the thick Plexiglas container in which the tissue was contained — and could do so using as little light as possible, so as to not damage the cells. “We developed a new technology that allows us to go deeper than fluorescence microscopy,” Intes said. “It allows us to see, first, if the cells are growing, and then, if they respond to the drug.”
This technique, Intes said, could allow researchers to evaluate the effectiveness of multiple drugs at the same time. It is not yet realistic though, he points out, for studying the effectiveness of certain therapeutics on a person’s individual tumor because of the short time period in which clinicians often have to provide treatment.
Source: Rensselaer Polytechnic Institute
09.03.2020