Image source: University of Helsinki/Photo: Emmy Verschuren
News • Functional diagnostics
New assay could advance personalized cancer treatment
A new study from the University of Helsinki shows that cells that are freshly isolated from lung cancers can be used to create robust drug response data.
This approach can identify actionable or non-responsive treatments, illustrated by a case study in which the assay was used to guide the compassionate treatment of a patient.
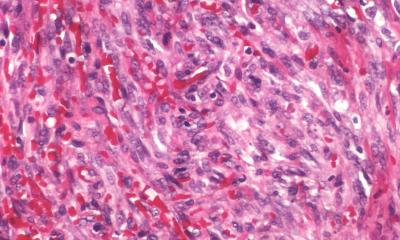
Each cancer tissue is unique, complicating treatment decisions. The power of precision medicine to match treatments to and individual patient is therefore evident. Yet, its actual success in the clinic has remained limited, particularly for solid tumors. Lung cancer is the most common cancer worldwide and has a poor prognosis compared to other cancer types. Based on genetic mutation analyses, matched treatments can be identified for around a third of patients with non-small cell lung cancer, but only just over half of all patients benefit from such gene-matched treatments. One of the issues is the lack of diagnostically interpretable assays that can identify the most promising treatment for a particular cancer. To overcome this challenge, a research team led by Emmy Verschuren from the Institute for Molecular Medicine Finland FIMM, University of Helsinki, validated an assay to enable drug response measurements in lung cancer samples immediately following surgery. Their promising approach has just been published in the journal Cell Reports Medicine.
[Tumor] tissue is extremely fragile, and biological changes are increasingly pronounced with time elapsed since the surgery
Emmy Verschuren
For patients with hematological malignancies, the FIMM precision cancer medicine efforts and collaborating teams have made great progress on matching individualized therapies to patients via the analysis of patient-derived blood samples. However, for solid epithelial tumors, these methods cannot simply be adopted. According to Dr. Verschuren, there still is a great need for robust diagnostic cell models since the presently available models take long times to be established, and importantly, do not guarantee the expansion of malignant cells. “We have invested many years of research to understand whether tumor tissue can be used to obtain reliable data. Not surprisingly, we learned that tissue is extremely fragile, and biological changes are increasingly pronounced with time elapsed since the surgery”, says Dr. Emmy Verschuren.
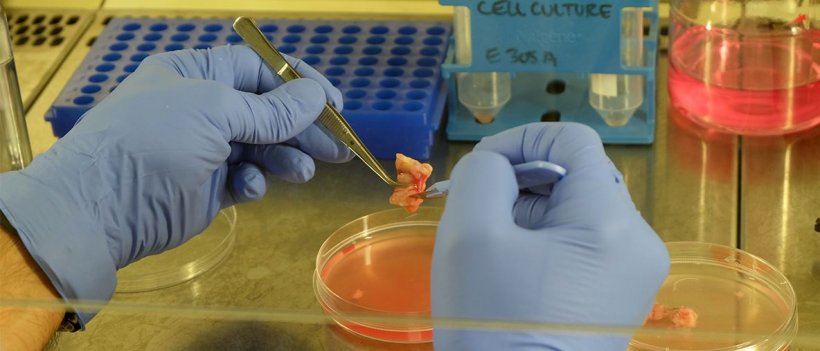
In their recent proof-of-concept study in collaboration with Professor Krister Wennerberg from the University of Copenhagen, her group aimed to develop an alternative approach to circumvent these challenges. The team set out to assess whether uncultured tumor cell populations could be used for drug profiling, immediately following their isolation. The research findings demonstrate the utility of what the researchers called Fresh Uncultured Tumor Cells, or FUTCs. The team tested the method by profiling twenty non-small cell lung cancer patient samples. The drug screening panel used contained 66 lung cancer-selective drugs. Their results demonstrated that robust drug response data was generated in 19 of 20 patient cases. Genetic cancer mutation analyses and the drug sensitivity data were well aligned, providing further support for the validity of the approach.
The promise of FUTC-based functional approach was also demonstrated via real-world translation, through compassionate treatment of a patient with refractory metastatic non-small cell lung cancer, per the patient’s request. The patient received clinical benefit from the treatment with three drugs selected based on the screening results. “The FUTC assay enables pharmacological testing of cancer cells in around 72 hours after sample collection and thus offers a possibility to impact treatment decision in the clinic, in an individualized manner”, says the first author of the study, Sarang Talwelkar from FIMM.
FUTC-based diagnostics could additionally help to predict clinical non-responses to highly-priced targeted therapies to decrease their considerable costs. “While it remains early days, and further investigation is warranted to test FUTC profiling on biopsies, we are hopeful that our assay can increasingly benefit patients with recurrent lung cancer”, says Dr. Verschuren. “In addition, it will be intriguing to see what we may learn by broader adaptation of the approach to other cancer types”, adds Prof. Wennerberg.
Source: University of Helsinki
18.08.2021