Image used with permission from: Graffy et al, Radiology 2019
Article • Imaging advances
Liver disease assessment: AI may give CT the edge over MRI
To assess diffuse liver disease, MRI is currently the modality of choice. New developments in artificial intelligence (AI) could tip the scales in favour of CT imaging. At ECR 2022 in July, experts showed how AI technology enables CT to quantify liver fat as exquisitely as MRI.
By Mélisande Rouger

Global fatty liver disease prevalence has reached an all-time high, with non-alcoholic fatty liver disease (NAFLD) affecting up to 25 to 30% of the population in the United States and Europe, according to recent studies.1 This calls for a necessary conversation between physicians, according to Prof. Peter Galle, Director of the Internal Medicine Department at the Johannes Gutenberg-Universität Mainz in Germany. 'The sheer numbers force us to talk about fatty liver,' he said as he opened the session. 'Fatty liver increases the chance of developing more serious diseases like fibrosis or hepatocellular cancer.'
One of the main issues for medical teams is that supportive biomarkers to prove the presence of fatty liver currently do not exist. The diagnostic process becomes a game of excluding every other underlying disease in every single case, which triggers the risk of overlooking patients, Galle explained. 'Hepatitis C is commonly associated with fatty liver, and if you haven’t had to screen the disease in a patient with fatty liver before, you might overlook it,' he said.
Detecting hepatocellular cancer (HCC) early on is another problem for hepatologists. 'We never really got into that in times where hepatitis B and C were prevalent,' he explained. 'We were lucky then, because these were relatively small groups of patients with a very high risk of developing HCC. With fatty liver, it’s the very opposite; we have a very large group and only moderate increase in HCC incidence. Screening and surveillance is even more of a problem.'
Assessing diffuse liver disease with AI-boosted CT
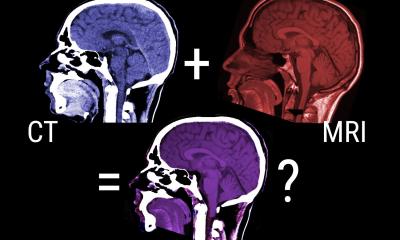
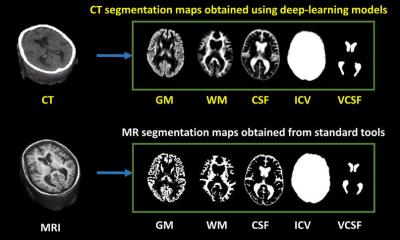
MRI has traditionally brought great results in quantifying hepatic fat, iron, and fibrosis – which are all key measurements to assess diffuse liver disease. But with the recent introduction of AI tools in CT imaging, radiologists are now exploring whether this modality could provide similar results much faster. 'It’s worth investigating because CT is done at such a high volume and we can also automate these measurements,' said Perry Pickhardt, chief of gastrointestinal imaging at the University of Wisconsin in the US. 'This option can also feed into an MR surveillance scheme with initial detection by CT.'
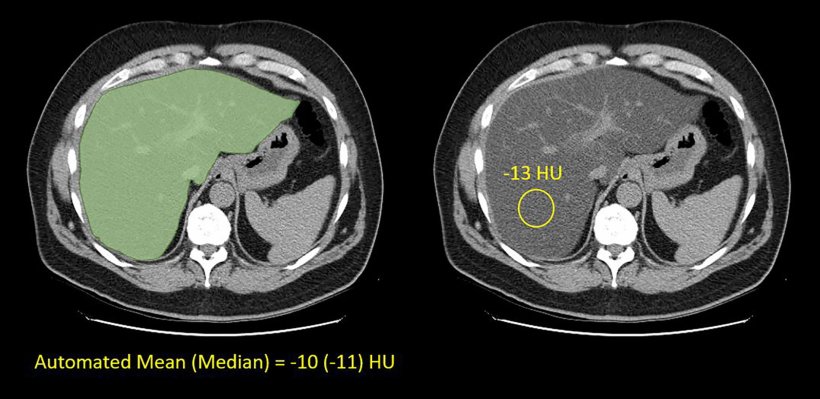
Pickhardt and his team have looked at hepatic steatosis with both CT and MR, comparing the performance of both modalities. 'We used unenhanced CT, which is more useful and effective at actual quantification of liver fat than enhanced scanning, and a phantom that was both MR and CT compatible and contained different levels of fat covering the entire spectrum from 0 to 100%,' he explained.
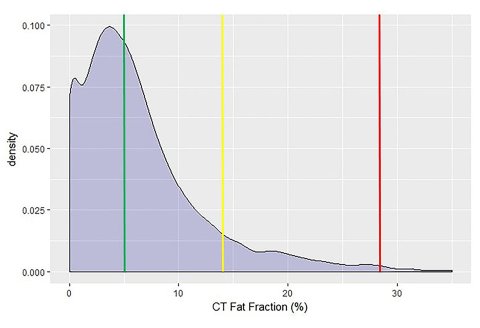
Image used with permission from: Graffy et al, Radiology 2019
The researchers found that there was a very nice linear correlation between Magnetic Resonance Imaging Proton Density Fat Fraction (MRI-PDFF) and unenhanced CT. 'That means we can convert from one to the other – i.e. start with CT and derive the equivalent MRI-PDFF value. Clinically, we can do things on the fly,' he said, adding that the results also apply to fibrosis assessment. Another study conducted in 400 healthy volunteers in Beijing showed a similar correlation between CT and MR.2
Radiologists can often tell if mild steatosis is present on ultrasound, but quantification remains difficult. 'There are emerging techniques in ultrasound, but they’re not at the level of what is done with CT or MR today,' he said. Prevalence of hepatic steatosis is rising, and based on ultrasound, estimated to be between 20-30% depending on the population. 'With CT measures and presumably MR in the same population, we find that about half the population qualify for at least mild steatosis,' Pickhardt said. 'But more importantly, we’d get about 10% qualifying for moderate or severe steatosis, which is becoming the main target.'
Incidental steatosis can be non-invasively detected and quantified with either CT or MR. AI-boosted CT could be very useful in predicting survival as well. Looking at a five-year curve, patients’ BMI provided no prognostic value, whereas liver fat qualification gave further insights in terms of predicting death. 'Liver and visceral fat does matter and non-contrast CT is quite good at showing these things. Since the number of CT scans is so great, we can actually do population-based opportunistic screening,' he said.
Profiles:
Perry J. Pickhardt is Chief of Gastrointestinal Imaging and Medical Director of Oncological Imaging at the University of Wisconsin School of Medicine & Public Health in Madison, WI, USA.
Peter R. Galle is Director of the Internal Medicine Department at the Johannes Gutenberg-Universität Mainz in Germany. He was CEO of Mainz Medical Center between 2005 and 2008.
References:
- Graffy et al.: Automated Liver Fat Quantification at Nonenhanced Abdominal CT for Population-based Steatosis Assessment; Radiology 2019
- Guo et al.: Liver Fat Content Measurement with Quantitative CT Validated against MRI Proton Density Fat Fraction: A Prospective Study of 400 Healthy Volunteers, Radiology 2019
01.11.2022