Article • Pros and cons of diagnostic techniques
Liquid biopsy vs. tissue biopsy: Getting the best of both worlds
Tissue biopsy and liquid biopsy can increasingly be used as complementary or alternative approaches, with advantages and limitations to each. While speakers at the recent 35th European Congress of Pathology in Dublin were quick to highlight that liquid biopsy was not about to replace tissue biopsy, the focus looked at the benefits and challenges of each through the lens of four expert speakers.
Report: Mark Nicholls

For his presentation, Professor Paul Hofman focused on the advantages and limitations of liquid biopsy versus tissue biopsy in thoracic oncology. In looking at how both biopsy techniques can be complementary, the Professor of Pathology and Head of the Laboratory of Clinical and Experimental Pathology at the Pasteur Hospital and Director of the IHU RespirERA, Nice, examined the landscape in thoracic oncology therapeutic decision making. Hofman further explored emerging biomarkers and molecular testing in thoracic oncology, provided insights on when and how to use tissue biopsy and liquid biopsy, and outlined recent developments of cf-DNA testing.
With more and more targeted genome alterations in thoracic cancer, looking for disease is a growing challenge, Hofman said. He emphasised the need to use NGS (next-generation sequencing) to address this. ‘We also need to consider what is not targeted; there is at least 40% of patients in Western countries without any genomic alteration with an associated drug, which is much too high.’ He underlined the importance of following ESMO (European Society for Medical Oncology) recommendations and guidelines but also noted that with some differences in US guidelines, there was a pressing need for global harmonization.
Emerging biomarkers call for complimentary approach
The benefits of using both liquid and tissue biopsy become evident in the context of emerging biomarkers, Hofman pointed out. Some of these markers are not detectable on liquid biopsy and may only be detected on tissue biopsy. ‘This is particularly true for an increased number of proteins, including some targets of antibody drug conjugates, which can be detectable and quantified only on tissue biopsy.’
With future and current biomarkers for non-small cell lung cancers (NSCLC), he advocated seeing tissue and liquid biopsies as complementary. ‘For our patients, we need to be sure about the right sample, so this is why now we need to think about the integration of liquid biopsy. Because sometimes it is a complementary approach but not an alternative approach if tissue biopsy is not available.’ While he pointed out that in the US, liquid biopsy was a first line approach, he suggested Europe was not yet at that stage.
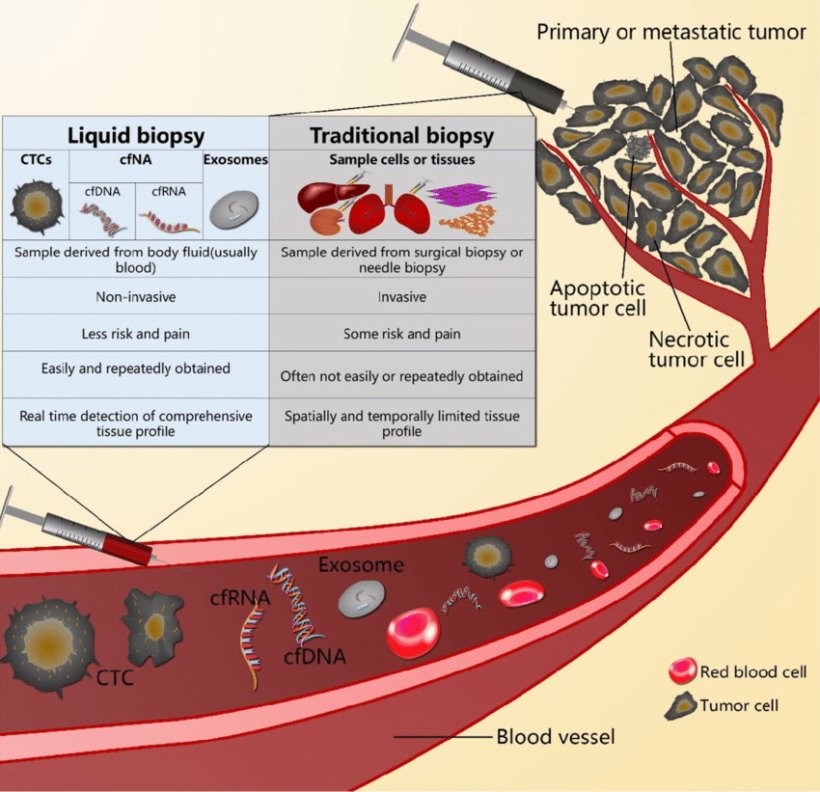
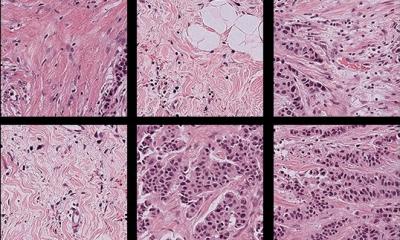
Image source: Qi ZH et al., J Cancer 2018 (CC BY-NC 4.0)
Mix and match to suit clinical needs
When dealing with lung cancer and the use of small tissue specimens, he felt blood specimens should be integrated into the process. ‘By tissue biopsy, we can see some mechanisms of resistance that we cannot see in liquid biopsy. For example, we know that expressions of some proteins are only on the tissue. ‘In tissue biopsy, gene amplification and detection of large gene deletion is probably higher than in liquid biopsy, but there are advantages of doing liquid biopsy, such as we do not need hospitalisation.’
He further pointed to technical, logistical, and biological issues and limitations that come with both approaches. Liquid biopsy is non-invasive, repeatable, can be done as an outpatient, and is cost effective but with no histological evaluation and cancer diagnosis. Turnaround time for tissue biopsy is always longer, creates the need for hospitalisation and is invasive, but offers histological evaluation, standardisation of workflow and sensitivity for fusions/amplification. ‘The best strategy is to match tissue and liquid biopsy at the same time,’ said Hofman.
Use cases and challenges in lung cancer
For advanced lung cancer, doing tissue and liquid biopsy provides an opportunity to increase detection of actual genomic alterations and create global molecular portraits of the tumours. This can increase the number of target possibilities, though he pointed out concordance was around 70%. ‘If we have negative results on tissue, then we have to look at the liquid biopsy results and vice versa,’ he added.
Additional challenges for integration of liquid biopsy in thoracic oncology include screening and the detection of minimal residual disease and when post-surgery to take the blood sample, but there is still a gap in introducing that into daily practice, the expert reported.
Tissue exhaustion becomes a growing challenge
To avoid tissue exhaustion, he said NGS should be performed in-house as sending samples outside the lab will not be sustainable in the near future.
Against a backdrop of current and emerging biomarkers, Hofman concluded: ‘We need to work hand in hand for tissue biopsy and liquid biopsy because we have more and more biomarkers to look for with less and less tissue, so we need to avoid tissue exhaustion. If there is tissue exhaustion, we can switch rapidly to liquid biopsy.’ However, he warned that as the next generation of pathology emerges, there is a need to be aware of false negative results in liquid biopsy.
Profile:
Paul Hofman is a Professor of Pathology and Head of the Laboratory of Clinical and Experimental Pathology at Pasteur Hospital, and Director of the IHU RespiraERA, Nice, France. His research focuses on lung cancer, including molecular pathology, biomarkers, and diagnostics. He is also investigating next-generation sequencing approaches to link personalised medicine and molecular biology.
27.05.2024