Article • Precision medicine
Liquid biopsy: the ‘next frontier’ for cancer detection?
Mark Nicholls reports from the National Cancer Research Institute (NCRI) virtual Festival, with four expert speakers discussing the role of liquid biopsy in cancer detection.
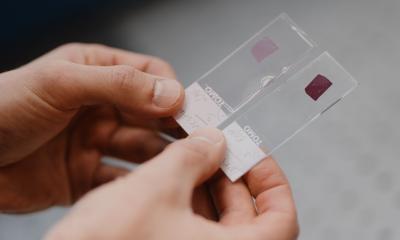
Liquid biopsy is playing a rapidly growing role in earlier detection and precision medicine in cancer. While blood- and urine-based biopsies offer researchers detailed molecular insights into cancer biology, the field is also moving towards clinical applications that directly benefit patients.

Four eminent speakers discussed the latest developments in the session “Liquid biopsy for cancer early detection and precision medicine - on and beyond circulating protein and DNA” at the National Cancer Research Institute (NCRI) virtual Festival in November. With research beginning to show the potential of liquid biopsies and first trials being launched, the session covered the different types of liquid biopsies, new developments, future perspectives, and current technologies such as the Galleri test developed by US company Grail. Hosted and chaired by Professor Klaus Pantel from University Medical Center Hamburg-Eppendorf and the University of Hamburg, Germany, it also examined the potential roles of liquid biopsy biomarkers for cancer management, with a forward-looking view of how to implement that into clinical practice.
Professor Pantel said: ‘For more than 10 years now, circulating DNA, circulating tumour cells, extracellular vesicles and other analytes have been used for detection and characterisation of tumour evolution and cancer screening in patients. Most of the studies have focused on analytes of blood samples but also additional fluids such as urine.’
Advantages over conventional biopsies

Outlining the clinical need of liquid biopsy, Professor Caroline Dive, from the Cancer Research UK (CRUK) Manchester Institute’s Cancer Biomarker Centre at the University of Manchester, said the indications for liquid biopsy in managing cancer patients are rapidly increasing: ‘This started with detection of specific mutations that predict targeted therapy response – selecting patients for EGFR inhibitors based on ctDNA EGFR mutations are an obvious example – but there are now further uses of liquid biopsies beyond predictive biomarkers being studied.’
Other areas of focus are minimal disease monitoring, for example, examining whether liquid biopsy can help assess more quickly whether there is tumour recurrence after surgical resection. Professor Dive added that ‘sensitivity and specificity of liquid biopsies, such as methylated ctDNA, may also find very early-stage tumours in patients.’
Liquid biopsy circumvents several of the challenges that conventional tumour biopsy faces; it is easier to repeat to monitor tumour progression, to determine developing treatment resistance in patients and to gather indications for therapy switching. The expert added: ‘Despite the excitement in the field, we need to be aware of the need to run really well-designed, well-powered, randomized controlled trials to show that liquid biopsy for the specific questions we seek to address, results in benefit to the patient.’
State of affairs for ctDNA analysis

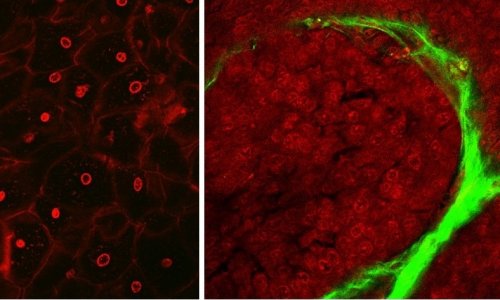
Dr Nitzan Rosenfeld from the CRUK Cambridge Institute, who leads a research group focussing on circulating tumour DNA (ctDNA) technology development, discussed the current view of ctDNA. He reported on tremendous progress in the application of ctDNA analysis methods for cancer, especially in advanced cancers. According to the expert, ctDNA-based analysis is rapidly entering clinical use with multiple roles including for molecular stratification. Progress with application of such methods for earlier cancers has been driven by the ability to analyse specific point mutations and genomic alterations that are present in the cancer with greater breadth and sensitivity. ‘The advantage of these cancer mutations is that they make for very highly-specific markers because you do not find them in the normal tissues,’ he added. However, a limitation of looking at cancer-specific mutations or alterations lies in the number of recurrent mutations.
A range of different approaches are employed to analyse signals genome-wide, with a notable example being Grail’s Galleri test, which looks across large stretches of the genome for methylation patterns. The promising assay is currently being rolled out as a large trial. ‘In molecular residual disease, we are now pushing sensitivity further and also detecting patients who are likely to relapse after treatment for early-stage cancer,’ Dr Rosenfeld said. ‘Earlier detection of cancer is the next frontier.’
Circulating tumour cells: Obvious potential, but…

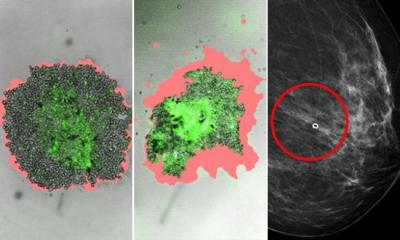
Meanwhile, Professor Yong-Jie Lu, from the Queen Mary University of London, discussed current developments in Circulating Tumour Cells (CTCs) as biomarkers, highlighting pros, cons and technical challenges.
Although the exploration of ctDNA for biomarkers has progressed significantly in the last decade, research in this field started much earlier and has been investigated for two decades. ‘We know that cancer metastasis/spread is responsible for the most of cancer death and CTCs are the seeds of cancer metastasis,’ Professor Lu explained. ‘Their potential as biomarker for aggressive cancer is obvious.’ He noted that CTCs are detectable at a very early stage of cancer development. This has been shown in breast, lung and prostate cancer, and should be applied to other cancers as well. ‘CTCs can also be analysed cell-by-cell to determine inter-cellular heterogeneity, which is impossible for circulating or urine DNA and RNA analysis. They can also be cultured for in-vitro drug sensitivity testing to guide treatment selection, similar to bacteria antibiotics sensitivity tests.’
Despite this, transfer of CTCs to clinical application is progressing much slower than ctDNA, for various reasons: Since CTCs only make up a small part in blood samples, enrichment is required for analysis; and while analysing cells gives more additional information, it is more difficult than detecting rare molecules such as proteins and nucleic acid. Professor Lu concluded that efficient, simple and automated detection systems are required for the potential of CTCs as biomarkers to be fully realised. ‘In addition to products released from cancer cells, including cancer proteins, ctDNA and CTCs, other non-cancer cells and molecules released by them in the blood circulation also have the potential to be developed into cancer biomarkers for cancer diagnosis, such as white blood cells and platelets. These are much more abundant in blood samples, and so are detected much easier.’
Urine biomarkers: the ‘ultimate health monitoring tool’?

Professor Tatjana Crnogorac-Jurcevic, from Barts Cancer Institute in London, focused on the pros and cons of urine as a biomarker source, compared to blood-based biomarkers. ‘Urine has obvious advantages,’ she said. ‘In contrast to blood, urine can be sampled completely non-invasively in large volumes and repeatedly, and is amenable to self-sampling.’ Additionally, urine is arranged in a much less complex matrix – an important benefit for performing analyses in search of viable biomarkers. Its metabolic inertia is another advantage of urine over blood. ‘Yet, as urine is an ultrafiltrate of blood, with sensitive enough techniques we should be able to detect in urine most, if not all, biomarkers that are present in blood,’ the pathology expert explained. Her team had capitalised on these advantages in detecting mutations in urine, and successfully performing proteomics and microRNA profiling. ‘But a major drawback in urine is that some of the analytes are found in lower concentrations than in blood, particularly nucleic acids,’ she said.
Professor Crnogorac-Jurcevic explained that thus far, urine has mostly been utilised for discovery of biomarkers in uro-genital cancers, though urinary biomarkers have also been found in other cancers, such as lung, breast, colorectal and brain cancers. The focus of her research is to find biomarkers for early detection of pancreatic cancer and a panel of three proteins discovered in her laboratory – UroPanc – has now been taken into clinical trial. ‘The immediate future lies in a multi-analyte approach, but we would like to see early detection of various, if not all, cancers using a combination of various types of analytes. However, while I see urine and urine biomarkers as tools for disease detection and monitoring, I could envisage urine as an ultimate health monitoring tool,’ she concluded.
Profiles:
Professor Tatjana Crnogorac-Jurcevic is Professor of Molecular Pathology and Biomarkers at the Centre of Cancer Biomarkers and Biotherapeutics at Barts Cancer Institute at Queen Mary University of London. A major interest of her laboratory is pancreatic cancer, and her group is developing tests for early detection of this malignancy in urine.
Professor Caroline Dive is Director of the Cancer Biomarker Centre at Cancer Research UK’s (CRUK) Manchester Institute at the University of Manchester, with research spanning tumour biology, preclinical pharmacology, biomarker discovery, biomarker assay validation and clinical qualification to regulatory standards, bioinformatics, biostatistics and most recently, digital clinical trials. She is President of the European Association for Cancer Research.
Professor Yong-Jie Lu is a Professor in Molecular Oncology at Barts Cancer Institute, The Barts and London School of Medicine and Dentistry and the Queen Mary University of London. His liquid biopsy research focuses on circulating biomarker studies, in particular CTCs, aiming to translate them into cancer diagnosis, prognosis and therapeutic stratification.
Dr Nitzan Rosenfeld is a Senior Group Leader at the Cancer Research UK (CRUK) Cambridge Institute and a recognised leader and pioneer of the field of liquid biopsies in cancer. The group’s research helped establish applications of ctDNA for the study of cancer evolution, and for minimally invasive cancer diagnostics including molecular stratification, monitoring, and detection of residual disease.
Professor Klaus Pantel is chairman of the Institute of Tumour Biology at the University Medical Center Hamburg-Eppendorf and a pioneer in the field of cancer micrometastasis, circulating tumour cells and circulating nucleic acids. He introduced the term ‘liquid biopsy’ together with his colleague Catherine Alix-Panabieres and is founder and chairman of the European Liquid Biopsy Society (www.elbs.eu).
28.12.2021