Article • New EU regulation
Lab tests: Watch out! Conflict ahead
In May 2022 a shortage of several lab tests may come as many manufacturers struggle to comply with EU regulation requirements covering in vitro diagnostic medical devices (IVDR, Regulation (EU) 2017/746). Even modified tests and laboratory-developed tests will present a problem for hospitals and labs as explained by Dr Thomas Streichert, Private Docent and Director of the Institute of Clinical Chemistry at the University Hospital Cologne, Germany.
Interview: Daniela Zimmermann, Text: Michael Krassnitzer
HiE: In about six months, the EU regulation on in vitro diagnostic medical devices (IVDR) will apply. Lab managers, as well as experts in laboratory medicine, severely criticised the regulation. What are the problems?

Streichert: ‘In the worst case scenario next year many tests with CE mark that are currently used in labs and hospitals will no longer be available. We are facing a difficult situation and a major challenge for the healthcare system.’
What are the critical issues in IVDR?
‘IVDR contains many aspects that I consider important and correct: increased patient safety, classification of products according to risk, harmonisation of the conformity assessment procedure, supervision of the so-called notified bodies, harmonisation of the EU regulatory framework, or quality standards for products manufactured outside the EU. Another issue I find very positive: In the future, clinical tests will be reviewed for clinical performance. That means each new test that’s launched has to demonstrate its clinical value in performance evaluation studies, for example enhancement of a therapy.’
Where’s the hitch?
‘First, the time frame for implementation is rather short. The regulation came into force in 2017 and will apply as of 26 May 2022. While this transition period might sound long, it has turned out to be very ambitious, in view of the infrastructure that must be established for the future approval of in vitro diagnostic devices. Moreover, a precondition for the regulation, the central data base EUDAMED, is not yet fully operational.
‘In addition, there’s a problem with the notified bodies that need to be involved in the conformity assessment of critical products: after Brexit there were only six rather than 18 notified bodies left in the EU. This creates a bottleneck that slows down the process.’
According to a recent study under IVDR, a notified body has to be involved in about 78% of the approval procedure for in vitro diagnostic medical devices – up from previously 8%.
‘You are referring to a MedTech Europe study which is quite enlightening in many aspects: it shows the substantial risk that, next year, many tests will no longer be available. Particularly for rare diseases there are tests which are distributed by very small enterprises, often university spin-offs. For them, continuing to offer these tests might financially not be viable due to the high costs. If a manufacturer can no longer sell his tests as a CE-marked product, the test is still available on the market but the lab manager who purchased it has to validate the test and can be held liable. But validating a purchased test is pretty close to impossible.’
We understand that tests developed by the labs themselves will also face difficulties. Can you explain the problems?
It might well happen that we have to discontinue using this test even though it is useful for the patients
Thomas Streichert
‘A university hospital uses on average 700 to 800 laboratory-developed tests – so-called LDTs. In the future, all these in-house tests will have to comply with IVDR standards. This means a lot of work for hospitals and labs. The most problematic assays, in my opinion, are modified tests – i.e. commercially available assays where the labs deviate from the manufacturer’s protocol, for example by using the test with a different matrix.
‘At the University Hospital Cologne we measure a certain tumour marker in CSF, not in serum or plasma as the manufacturer prescribes. Strictly speaking this is a significant modification, which means we are considered the manufacturer of this product. Consequently, we have to validate this test ourselves. However, to do so we’d need the technical details of the assay, for example where the antibody binds, and we’d need access to the relevant performance tests. This is not only a time-consuming task but also requires the manufacturer to disclose this information. It might well happen that we have to discontinue using this test even though it is useful for the patients.’
Recommended article

Article • Mass spec, qPCR and more
Newborn screening: early detection – new diagnostic possibilities
Since its introduction around 60 years ago, the screening of newborn babies for immune, hormone and metabolic disorders has prevented many people from experiencing severe disease progression. The scope of systematic early testing has been significantly enhanced through mass spectrometry (MS). In our interview, Professor Uta Ceglarek, one of the driving forces behind the introduction of MS…
Could manufacturers adapt the intended purpose of their tests?
‘Manufacturers are not keen to do that. They are currently busy making their tests IVDR-compliant by the deadline. If they modified the intended purpose they would also have to go through the conformity assessment procedure again.’
There are also concerns that, in the future, labs will have to pay for tests that they themselves developed, but that are being distributed by an external company. Are these concerns justified?
‘At the University Hospital Cologne we use a number of mass spectrometry assays which we developed ourselves to measure medication levels. Today, a company is offering one of these tests in its product portfolio. If we want to comply with IVDR requirements with regard to the so-called industry privilege, we have to clinically and technically validate the assay that we developed ourselves against the commercially available test. If the latter is as good as or better than our own test, then we have to discontinue using our test and purchase the commercial assay. But why should we use scarce resources to develop a test which two years down the road will be offered by a company and we will be forced to buy it?’
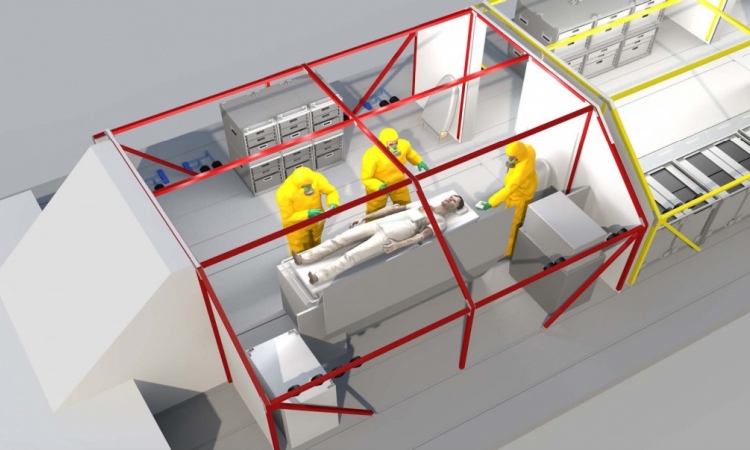
Image source: Shutterstock/angellodeco
How can this problem be solved?
‘By defining the intended purpose for the patient groups very narrowly and, at the same time, highlighting the benefits, e.g. useability in other matrices such as CSF. Even when we use a smaller sample than indicated by the manufacturer, our test is still better because it’s better for the patient – less blood has to be drawn. Thus I’m not too worried about the industry privilege. I think it will be rather unlikely that a manufacturer will insist on us using his test and threatening litigation. In order to do so he would have to show that his assay fully complies with the quality requirements of our in-house assay. That means he would have to disclose his development processes – which he rather wants to avoid.
‘The pressure is not applied by the manufacturer but by the regulatory body. In general, the number of LDTs used will be much smaller.’
Will this have financial consequences?
During the pandemic, imagine if we would have had to wait for commercial manufacturers to offer Covid-19 tests
Thomas Streichert
‘In-house developments are often significantly cheaper for labs. However, the comments on IVDR point out that economic considerations must not be the reason for the use of LDTs. Thus, the hospitals have no incentive any more to develop their own tests. In the long run this will impair the ability of hospitals and labs to react in acute situations. During the pandemic, imagine if we would have had to wait for commercial manufacturers to offer Covid-19 tests.’
What other difficulties will labs and hospitals have to face in the wake of IVDR?
‘The term in vitro diagnostic device was expanded to include software. While this is only one line in the regulation, it has immense consequences: software developers have to meet the same requirements as the manufacturers of lab products. In Next Generation Sequencing, human genetics or molecular tumour diagnostics labs use complex software solutions that integrate several test results. All these software solutions must be reviewed to make sure they are not lab-developed items under IVDR. Hardly anybody has ever validated software – much less validated for IVDR conformity.’
How can this issue be navigated?
‘I am chair of a sub-group in the Working Group of Scientific Medical Societies (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften – AWMF), which deals exclusively with software issues in the context of IVDR. We compiled a guidance document for all those who develop such software solutions. After all, IVDR is not overly specific with regard to software, which gives us some room to manoeuver. But the requirements exist and must be complied with. At the end of the day we will have to jump through that hoop.’
Profile:
Dr Thomas Streichert is Director of the Institute for Clinical Chemistry, Medical Director of the Centre for Laboratory Diagnostics (Clinical Chemistry, Microbiology, Virology, Pharmacology, Endocrinology) and Interim Director of the Institute of Pharmacology, Therapeutic Drug Monitoring, at the University Hospital Cologne. Born in South Africa, Streichert studied medicine in Hamburg where he also worked as junior physician and consultant. In 2013, the specialist physician for laboratory medicine joined the University Hospital Cologne. He is chair of the E-Learning Commission at the University Hospital Cologne and member of the German Society for Clinical Chemistry and Laboratory Medicine (Deutsche Gesellschaft für Klinische Chemie und Laboratoriumsmedizin e.V.).
15.11.2021