Image source: UChicago Medicine; photo: Julian Romano
News • Intraoperative imaging
New iMRI tech to make brain surgery safer, faster and more precise
Transformative technology integrates functional monitoring with surgical treatment
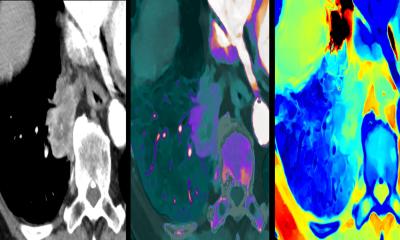
A new intraoperative MRI (iMRI) system promises to make complex neurosurgeries safer, faster, and more precise — performing functional MRI scans in real time during surgery and helping surgeons detect potential complications in as little as seven seconds. The University of Chicago Medicine, one of the first hospitals in the US to utilize the technology, reports significant benefits for both patients and surgical teams.
With real-time imaging, doctors can tailor their approach. They can shift care from simply removing visible lesions to treating a patient's underlying disease biology based on the metabolic profiles and brain networks involved, said Peter Warnke, MD, a neurosurgeon and Director of Stereotactic and Functional Neurosurgery at UChicago Medicine.

Image source: UChicago Medicine; photo: Julian Romano
The iMRI also saves time and reduces risk. Until now, patients undergoing complex neurosurgery often had to be stabilized and transported several floors away for imaging mid-procedure, adding risk and extending surgery times. With the new iMRI suite located directly between two operating rooms in the Center for Care and Discovery, surgeries can be reduced by one to two hours, improving safety and recovery for patients. Having the two dedicated operating rooms also allows surgeons to perform more complex cases in a day.
Intraoperative MRI is a critical technology in surgery of the brain and spine to treat complex neurosurgical disease
Mohamad Bydon
Mohamad Bydon, MD, Chair of the Department of Neurological Surgery at UChicago Medicine and health system leader for Neurological Surgery, said the iMRI — primarily used for patients with brain tumors, epilepsy, vascular disease of the brain and complex spinal conditions — is not just another imaging tool. Rather, he calls it a transformative technology that integrates functional monitoring with surgical treatment.
“Intraoperative MRI is a critical technology in surgery of the brain and spine to treat complex neurosurgical disease,” Bydon said.
The iMRI investment strengthens UChicago Medicine’s ability to provide world-class brain, spine, epilepsy and vascular surgeries close to home, while also attracting patients from around the country and the world, Bydon said. The iMRI investment strengthens UChicago Medicine's ability to provide world-class brain, spine, epilepsy and vascular surgeries, added Jeffrey B. Matthews, MD, Surgeon-in-Chief for the University of Chicago Health System and Chair of the Department of Surgery.
Source: University of Chicago Medical Center
10.02.2026