News • PET-scan
Imaging agent helps predicting lung cancer therapy success
With the help of a new radioactive tracer, doctors can predict with more than 80 percent accuracy how well a widely-used lung cancer drug will combat tumors, according to researchers at Stanford.
Doctors contemplating the best therapy for lung cancer patients may soon be able to predict the efficacy of a widely used lung cancer drug based on an imaging agent and a simple scan, according to the findings of a new clinical trial co-led by researchers at the Stanford University School of Medicine.
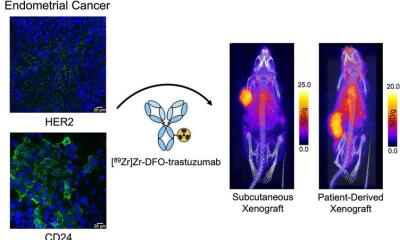
The researchers developed a PET scan-compatible imaging agent engineered to seek out a specific mutation found in nonsmall cell lung cancer (which accounts for about 80 percent of lung cancers), bind to it and emit a radioactive signal that flags its presence. Patients whose tumor sites don’t emit the tracer’s signal while undergoing a PET scan likely don’t harbor the mutation, and can be spared the treatment. In addition to exposing the molecular roots of tumors, the imaging agent reveals potential weak spots in the cancer where specific therapeutic drugs can be administered to counteract the pro-tumor mutation.
‘Like a full-body biopsy’
One way to think about this imaging technique is like it’s taking a biopsy of the entire body, and that gives a much more complete picture of the mutational status of the primary tumor, which allows you much better information to treat the cancer.
Sam Gambhir
As with many cancer-imaging agents, the new tracer, called F-MPG, works with a PET scan. While there’s no shortage of PET scan tracers, Sanjiv “Sam” Gambhir, MD, PhD, professor and chair of radiology at Stanford, likens the development of these imaging agent to the development of drugs. “There are hundreds of drugs, just like there are hundreds of imaging agents; we have to keep building new ones for different purposes,” he said. “We have to keep looking for different ways to interrogate the underlying biology of the tumor, and the new method we’ve developed goes after actually measuring mutations in the tumor.”
Most PET scans use a tracer that can only tell if a tumor is active in terms of its metabolism. In this case, F-MPG can tell doctors whether the tumor cells are present and whether they contain a mutated version of a protein called epidermal growth factor, which when overexpressed spurs cell division. The F-MPG tracer floats throughout the body, glomming onto any mutated epidermal growth factor proteins. Once latched on, it emits blips of detectable energy in the form of gamma rays, revealing the location and mutational details of the culprit protein.
“If the PET scan shows a high signal from the tracer in a patient’s lung cancer, that’s predictive of someone who is going to respond well to the specific epidermal growth factor therapy,” Gambhir said. “For those who show low signals, they’re likely not going to respond, so you need to look into other treatment options.”
Gambhir points out that biopsies, or a sample of the tumor, can also tell doctors what mutations are present. But tumors are so complex that a single biopsy may not accurately capture the spectrum of mutations present in the mass, and it’s even less likely to characterize the mutations present in multiple tumors including those that have spread throughout the body. “One way to think about this imaging technique is like it’s taking a biopsy of the entire body, and that gives a much more complete picture of the mutational status of the primary tumor, which allows you much better information to treat the cancer,” Gambhir said.
Guided by the glow
At Harbin Medical University, members of the research team conducted a 75-participant clinical trial with the tracer, monitoring which tumors lit up (or had a high signal) on a PET scan and which had a low signal. Among the participants whose tumors appeared with the help of the tracer — meaning their tumor cells had the epidermal growth factor mutation — more than 80 percent saw a positive response from the targeted drug: Either their tumors shrank or tumor growth slowed. In contrast, only 6 percent of participants who lacked PET scan evidence of the mutation benefited from the drug.
Gambhir noted that the clinical trial was the first time this tracer had been used in humans. The next stage of the research, he said, is to recruit more participants for an even larger trial and, barring unexpected complications, eventually use the tracer’s data to guide treatment plans for lung cancer patients. Currently, the tracer is only approved for use in China, so the studies will continue at Harbin. “We’d like to continue to build our collaboration with the terrific group at Harbin, and work toward a clinical trial network in China for testing many different tracers,” he said.
Source: Stanford Medicine
09.03.2018