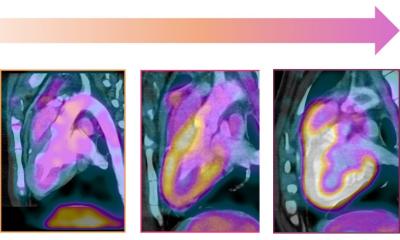
Image courtesy of the Sharma Lab at Cedars-Sinai
News • Chemotherapy and cancer drugs
‘Heart-on-a-Chip’ to test cardiotoxicity of treatments
Cedars-Sinai stem cell researchers poneer new technology to test chemotherapies and other cancer drugs for heart toxicity
In a study published in the peer-reviewed journal Lab on a Chip, they show that the heart-on-a-chip, created using stem cells, accurately predicts the effects of drugs on human heart cells.
The investigators worked with induced pluripotent stem cells, which are blood cells that have been reprogrammed into stem cells and can be turned into any cell type in the body. They used the stem cells to create two types of heart cells, but instead of placing them all together in an unstructured cell culture dish, as is usually done in heart toxicity testing, the investigators introduced the cells into specialized chips.
If a patient with cancer might receive a treatment that could have adverse effects on their heart, we can create induced pluripotent stem cells from a small sample of their blood
Arun Sharma
The 3D chips feature two channels that are arranged to cross each other, keeping each cell type separate but allowing them to interact. The chips also allow for movement and the introduction of fluids. “We grew heart muscle cells and blood vessel cells,” said Arun Sharma, PhD, a research scientist in the Board of Governors Regenerative Medicine Institute, Smidt Heart Institute, Cedars-Sinai Cancer, and the Department of Biomedical Sciences at Cedars-Sinai and senior author of the study. “The chip allows us to stretch the cells back and forth to mimic a heartbeat, and to introduce fluid to mimic the flow of blood through the heart. It’s like giving the cells a workout that strengthens the muscle cells and allows the vessel cells to form mini blood vessel-like structures.” These “matured” cells provide a better test platform for drug toxicity studies than cells that haven’t undergone this maturation process because they more closely resemble the way adult heart cells function, Sharma said.
To demonstrate the proficiency of heart-on-a-chip as a drug-testing platform, the research team, including lead author and postdoctoral fellow Maedeh Mozneb, PhD, subjected the heart chip to a chemotherapy drug called a VEGFR/PDGFR-inhibiting tyrosine kinase inhibitor, which is known to have adverse effects on heart muscle and blood vessel cells. Damage was observed to both cell types in the heart chips.
If future studies continue to show good results, heart-on-a-chip technology could significantly reduce drug development costs and improve the rate at which new therapies become available.
Another future possibility for these heart chips is the creation of patient-specific chips to personalize cancer treatment. “If a patient with cancer might receive a treatment that could have adverse effects on their heart, we can create induced pluripotent stem cells from a small sample of their blood,” Sharma said. “We can turn those stem cells into heart muscle and blood vessel cells and put them on a chip that will serve as a personalized avatar for how that person’s heart might react to the treatment. This is one of the most exciting applications of this technology, truly advancing personalized medicine at Cedars-Sinai.”
Also a possibility: Taking these chips beyond a single organ. “We eventually hope to bring our various organ models together,” said Clive Svendsen, PhD, executive director of the Board of Governors Regenerative Medicine Institute and co-author of the study. “My lab has been fine-tuning this technology to help us develop models of neurological diseases, and other labs in our institute have been working on chips for the liver and the gut microbiome. Bringing all of these chips together to create a ‘patient-on-a-chip’ model is part of our long-term vision for precision medicine.”
Source: Cedars-Sinai
06.02.2024