Healthcare economics
A study from the United Kingdom raises questions over the cost-effectiveness of breast screening
Research using an analytical health economics model has suggested the current system of screening within the UK’s National Health Service (NHS) is only moderately likely to be cost effective.

However, Prof. Paul Pharoah and team, from the University of Cambridge, also highlighted the lack of relevant data currently available to reach clear conclusions and indicated significant further primary research will be needed for cost effectiveness studies to provide definitive data to inform policy.
The study followed last October’s report from the Independent UK Panel on Breast Cancer Screening, which highlighted the need for a cost effectiveness study.
Using a life table model to generate an imaginary cohort of women, researchers simulated what happens to women year by year from the age of 50 over a period of 35 years, factoring in screening history, breast cancer diagnosis and mortality and mortality from other causes to compare the two and examine benefits and costs.
Professor Pharoah: ‘The model depends on a whole series of input parameters, such as how effective breast cancer screening is in reducing breast cancer mortality and what the size of the over diagnosis is. All those parameters are estimated with some uncertainty so in a sense there is no single result of the model but part of the purpose of doing this was to try and get a feel of how important that uncertainty actually was.’
Their base case scenario estimated that breast cancer screening resulted in a small gain in quality adjusted life years (QALY) at a cost of £20,800 per QALY gain, marginally above the National Institute for Health and Clinical Excellence (NICE) threshold of £20,000 of QALY as representing good value for money.
New trials for long-term effects needed
Results suggest there were 1,521 fewer deaths from breast cancer and 2,722 over-diagnosed breast cancers but, over the 35 years, the model found the gain in survival was 9.2 days per person and 2.7 quality-adjusted days per person screened.
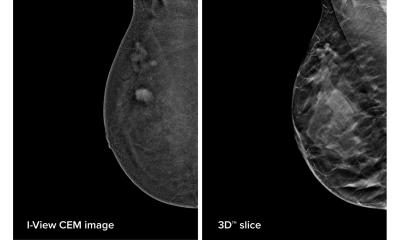
However, the study highlighted a ‘surprising lack of good data’ on the effectiveness of breast cancer screening using modern digital mammography, or on the long-term effects on the quality of life from screening.
Professor Pharoah said most screening trials were conducted 20-30 years ago using old techniques with little carried out using modern mammography, surgery and treatments. ‘We also have absolutely no idea what the long-term quality of life is of somebody diagnosed with breast cancer aged 50 who has had radiotherapy and a mastectomy. One of the problems of screening is over-diagnosis, so if you are over diagnosing breast cancer, how that affects long-term quality of life is important.’
The work, he added, highlights the fact that more information is needed and the study raises several questions. ‘You can’t say that screening is definitely a highly cost-effective intervention. Based on our results you’d not say it’s absolutely a “must” from a cost-effectiveness point of view, but you wouldn’t say it’s ridiculously expensive either.’
While screening does identify breast cancers, Professor Pharoah believes the NHS should offer women more information about the issue of over-diagnosis so they can make an informed choice about whether to opt for screening or not. ‘My view is that, because the randomised controlled trials of breast cancer screening are so old and based on old technology, a new and very large randomised controlled trial of breast cancer screening should be carried out.’
He thinks it unlikely that such a study will be conducted in the UK and while acknowledging his latest cost-effectiveness analysis may not in itself be a “game changer” he hopes it will help towards women being better informed about wider issues surrounding screening.
PROFILE
Paul Pharoah, Professor of Cancer Epidemiology at Cambridge University, qualified in Medicine at the University of Oxford in 1986. Following a series of internal medicine posts, in 1996 he became a research fellow in the CRC Human Cancer Genetics group. Gaining his doctorate in 1999, he won the Cancer Research UK Senior Clinical Research Fellowship, enabling him to develop an independent research programme. Major research focus: common genetic variation and breast and ovarian cancer susceptibility, the role of germline genetic variation in determining clinical outcome after a diagnosis of breast or ovarian cancer, and the molecular pathology of breast and ovarian cancer
05.07.2013