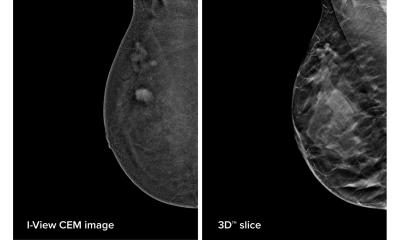
Image source: Conant et al., Radiology 2023 (© RSNA)
News • DBT vs. standard digital mammography
Huge study shows: Tomosynthesis better at breast cancer detection
In a study of over a million women, digital breast tomosynthesis (DBT) showed improved breast cancer screening outcomes over screening with standard digital mammography alone.
The results of the study were published in Radiology, a journal of the Radiological Society of North America (RSNA).
Breast cancer is the most common cancer among women in the United States. While breast cancer mortality has been on the decline since the late 1980s due to improvements in early detection and treatment, it still remains the leading cause of cancer death among women. The five-year relative survival rate of breast cancer when it is detected early in its localized stage is 99%, according to the American Cancer Society. Regular screening is the most reliable method for the early detection of breast cancer.

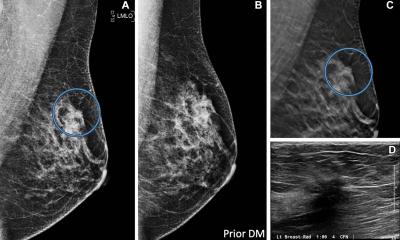
Image source: RSNA
Screening with two-dimensional (2D) digital mammography alone is still the standard of care at many sites, but it has its limitations due to its inability to detect some cancers. There is a growing amount of evidence that DBT, a more advanced technology, has a higher breast cancer detection rate due to its ability to capture multiple X-ray images of the breast from different angles rather than the typical single image obtained with a standard 2D mammogram. DBT is especially beneficial for women with denser breast tissue.
“The purpose of our study was to evaluate screening outcomes among a large cohort of women in the United States who were screened with either 2D digital mammography alone or with DBT,” said study co-author Emily F. Conant, M.D., FSBI, professor of radiology and chief in the Division of Breast Imaging at the Hospital at the University of Pennsylvania in Philadelphia.
For this retrospective cohort study, Dr. Conant and colleagues compiled data from five large health care systems across the United States. The study group consisted of over 1 million women aged 40 to 79 who were screened with either DBT or 2D digital mammography alone between January 2014 and December 2020. The screening outcomes such as cancer detection and false positive rates were compared across the two screening groups.
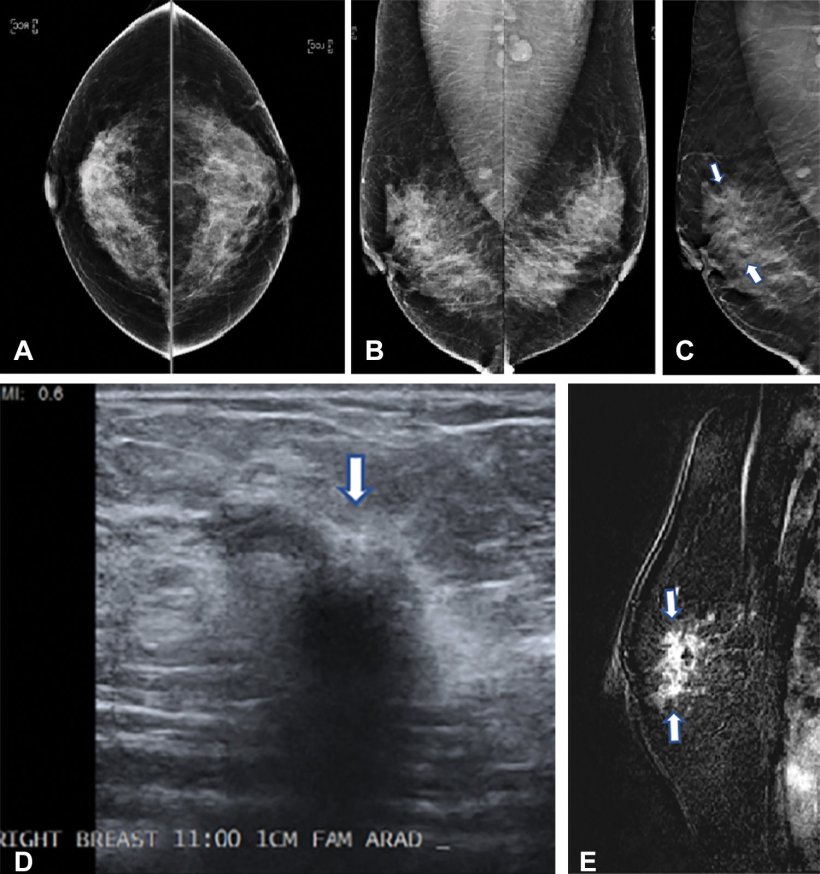
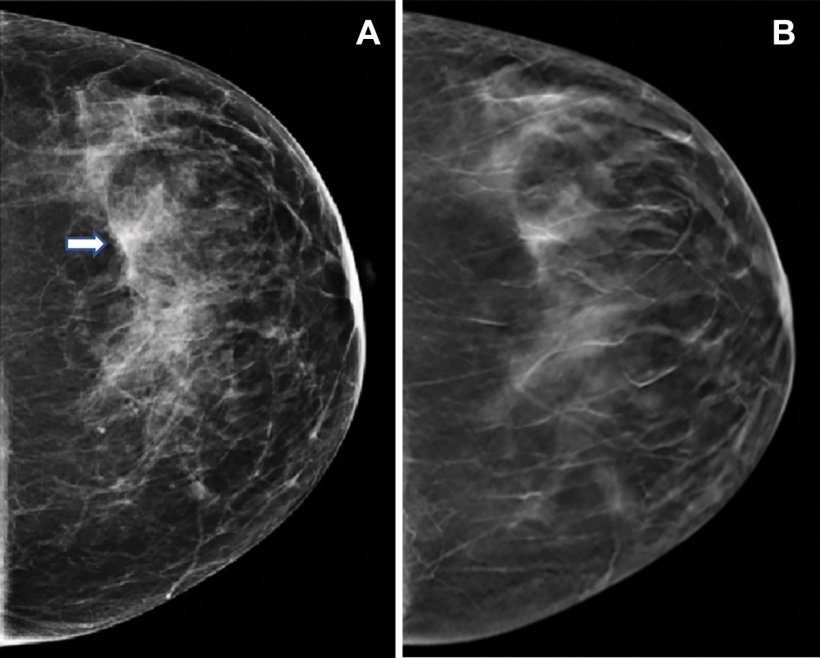
Image source: Conant et al., Radiology 2023 (© RSNA)
“This study was extremely large with most women having at least 2 screens resulting in over 2 million screening exams across five large and diverse health care systems,” Dr. Conant said.
Compared to 2D digital mammography alone, DBT was associated with important improvements in screening outcomes. The cancer detection rate for patients screened with DBT was higher at 5.3 per 1,000 screened, compared to 4.5 per 1,000 screened with 2D digital mammography only. DBT also had a lower rate of false positives and recalls from screening. “We showed that the most important mammographic screening outcomes, increased cancer detection combined with fewer false positives, were significantly improved when women were screened with digital breast tomosynthesis compared to 2D digital mammography alone,” Dr. Conant said. “Therefore, women should seek out sites that routinely offer breast cancer screening with DBT.”
Source: Radiological Society of North America
16.03.2023